Colorectal cancer stands as one of the most preventable yet deadly forms of cancer, ranking as the third most common cancer worldwide and the second leading cause of cancer-related deaths.
However, research demonstrates that up to 75% of colorectal cancer cases could be prevented through proactive health measures and lifestyle modifications.
Understanding how to protect your colorectal health involves a comprehensive approach that encompasses regular screening, strategic dietary choices, lifestyle modifications, and awareness of risk factors.
This guide provides you with evidence-based strategies to significantly reduce your risk of developing colorectal cancer while promoting optimal digestive health.
Read more: Health Screening in Singapore
Understanding Your Colorectal Cancer Risk Profile

Your individual risk for colorectal cancer depends on multiple factors, some within your control and others determined by genetics or age.
The overall lifetime risk stands at approximately one in 23 for men and one in 26 for women, but these numbers can vary significantly based on personal circumstances.
Age represents the most significant non-modifiable risk factor, with most cases occurring after age 50.
However, recent trends show increasing rates among younger adults, prompting updated screening guidelines that now recommend beginning at age 45 instead of 50.
Family history plays a crucial role in determining risk levels. Having a parent, sibling, or child with colorectal cancer doubles your risk, while certain inherited genetic conditions like Lynch syndrome or familial adenomatous polyposis can increase risk dramatically.
Personal medical history also influences your risk profile. Previous colorectal cancer, large polyps, ovarian cancer, or inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease all elevate your risk level and may require more frequent monitoring.
Related article: The Ultimate Guide to Losing Weight in Singapore
Comprehensive Screening: Your First Line of Defense
Regular screening represents the most powerful tool for colorectal cancer prevention.
Screening tests can detect cancer in its earliest, most treatable stages and identify precancerous polyps that can be removed before they develop into cancer.
Colonoscopy Screening
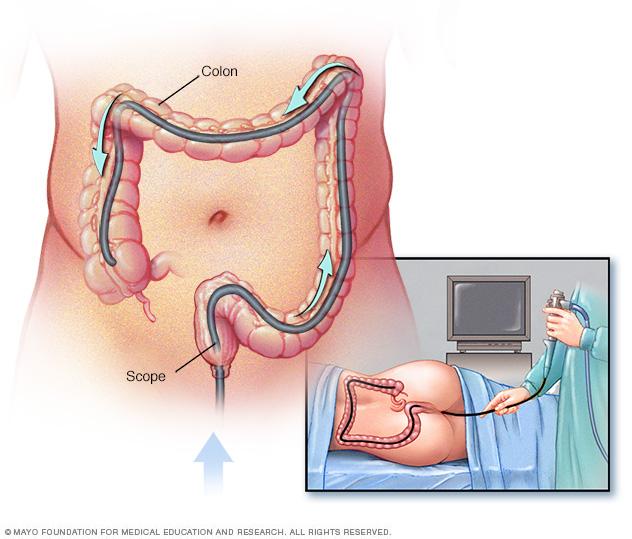
Colonoscopy remains the gold standard for colorectal cancer screening. This comprehensive examination allows doctors to visualize the entire colon and rectum while simultaneously removing any suspicious polyps discovered during the procedure.
The procedure involves inserting a flexible tube with a camera through the rectum to examine the full length of the large intestine. While sedation is typically used for patient comfort, the test provides the most thorough examination possible and serves both diagnostic and therapeutic purposes.
For individuals at average risk, colonoscopy screening should begin at age 45, with follow-up examinations every 10 years if results are normal. Those with elevated risk factors may need to start screening earlier and undergo more frequent examinations.
Read more: Comprehensive Guide to Colonoscopy in Singapore
Alternative Screening Options
Several effective alternatives exist for those who prefer different screening approaches or have specific medical considerations.
Home-based stool tests offer convenience and ease of use. The Fecal Immunochemical Test (FIT) and Fecal Occult Blood Test (FOBT) detect hidden blood in stool samples, which can indicate the presence of polyps or cancer. These tests require annual completion and, if positive, necessitate follow-up colonoscopy.
Stool DNA testing represents a newer approach that identifies both blood and genetic changes associated with cancer or polyps.
This test requires completion every three years and provides higher sensitivity than traditional blood-only tests.
Sigmoidoscopy examines only the lower portion of the colon but can be effective for detecting abnormalities in this region. This test typically requires completion every five years and may be combined with annual stool testing for comprehensive screening.
Read more: Best JB Health Screening Clinics for Singaporeans
Strategic Dietary Approaches for Colorectal Health
Your dietary choices significantly influence your colorectal cancer risk, with research consistently demonstrating that certain foods provide protective benefits while others increase risk.
Foods That Protect Your Colon
High-fiber foods form the foundation of a colon-healthy diet. Dietary fiber increases stool bulk, speeds waste movement through the colon, and promotes beneficial bacterial growth in the digestive system.
Adults should aim for 22 to 34 grams of fiber daily, depending on age and gender. Excellent fiber sources include whole grains such as brown rice, quinoa, barley, and oatmeal.
These foods provide not only fiber but also essential vitamins and minerals that support overall colon health.
You might like: Homeopathy in Singapore
Fruits and vegetables offer multiple protective compounds including fiber, antioxidants, and phytonutrients.
Non-starchy vegetables and fresh fruits should comprise a significant portion of your daily intake, with particular emphasis on leafy greens, cruciferous vegetables, and colorful produce.
Dairy products provide calcium and vitamin D, nutrients consistently associated with reduced colorectal cancer risk.
Low-fat milk, yogurt, and cheese offer these protective benefits while supporting overall nutritional needs. Research suggests aiming for 1000 to 1200 milligrams of calcium daily.
Legumes deserve special recognition for their dual benefits of high fiber content and plant-based protein.
Beans, lentils, peas, and soybeans provide essential nutrients while supporting digestive health and offering protective compounds against cancer development.
Essential Foods for Colorectal Protection
- High-fiber foods: Whole grains, vegetables, fruits, and legumes
- Dairy products: Low-fat milk, yogurt, and cheese for calcium and vitamin D
You might like: Best Yoga Classes in Singapore
Foods to Limit or Avoid
Red meat consumption requires careful moderation, as research links higher intake with increased colorectal cancer risk.
Limit red meat consumption to fewer than three servings per week, with smaller portions being even better for optimal health.
Processed meats pose an even greater risk than fresh red meat. Bacon, sausage, hot dogs, and deli meats undergo preservation processes that create potentially carcinogenic compounds.
The evidence linking processed meat consumption to colorectal cancer is particularly strong, warranting significant limitation or elimination from your diet.
This might help: Eating Disorder Treatment in Singapore: Causes, Recovery
High-temperature cooking methods can create harmful compounds in meat. Grilling, broiling, and pan-frying at high temperatures produce heterocyclic amines and polycyclic aromatic hydrocarbons, chemicals associated with increased cancer risk.
Consider gentler cooking methods like braising, steaming, or roasting at moderate temperatures.
Refined carbohydrates and added sugars contribute to insulin resistance and inflammation, potentially increasing cancer risk. Limit consumption of white bread, sugary snacks, and processed foods high in refined carbohydrates.
Essential Lifestyle Modifications for Protection
Physical activity provides powerful protection against colorectal cancer while offering numerous additional health benefits.
Regular exercise helps maintain healthy body weight, improves immune function, and may directly influence cancer-protective pathways in the body.
Exercise Recommendations
Aim for at least 30 minutes of moderate-intensity physical activity most days of the week. This can include brisk walking, cycling, swimming, dancing, or household activities like gardening or vigorous cleaning.
The type of exercise matters less than consistency and duration. Choose activities you enjoy to ensure long-term adherence to your exercise routine. Even light physical activity provides benefits compared to a sedentary lifestyle.
Recent research emphasizes the importance of reducing sedentary time in addition to increasing active time. Take regular breaks from sitting, use standing desks when possible, and incorporate movement throughout your daily routine.
Weight Management Strategies
Maintaining a healthy body weight significantly reduces colorectal cancer risk. Excess body weight, particularly around the midsection, is linked to increased risk of multiple cancers, including colorectal cancer.
Focus on sustainable weight management approaches that combine appropriate caloric intake with regular physical activity. Even modest weight loss can provide health benefits if you’re currently overweight.
Avoid extreme dieting approaches that are difficult to maintain long-term. Instead, focus on gradual lifestyle changes that support both weight management and overall health improvement.
Tobacco and Alcohol Considerations

Smoking cessation represents one of the most impactful changes you can make for your overall health, including colorectal cancer prevention.
Tobacco use is linked to increased risk of colorectal cancer and numerous other health conditions.
If you currently smoke, seek support for cessation through your healthcare provider, smoking cessation programs, or support groups.
The benefits of quitting begin shortly after your last cigarette and continue to accumulate over time.
Alcohol consumption requires careful consideration, as even moderate alcohol intake is associated with increased colorectal cancer risk.
The safest approach is to avoid alcohol entirely, but if you choose to drink, limit consumption to no more than one drink per day for women or two drinks per day for men.
Advanced Prevention Strategies and Special Considerations
Nutritional Supplements and Medications
Certain medications and supplements may provide protective benefits, though they should not replace healthy lifestyle choices and regular screening.
Aspirin use has shown promise in colorectal cancer prevention, with daily low-dose aspirin reducing cancer risk when taken for at least two years.
However, aspirin use carries risks including increased bleeding, so discuss potential benefits and risks with your healthcare provider.
Calcium and vitamin D supplementation may provide additional protection beyond dietary sources. Consider supplementation if your dietary intake is insufficient, but prioritize food sources when possible.
Non-steroidal anti-inflammatory drugs (NSAIDs) other than aspirin show potential protective effects in research studies, but they’re not currently recommended specifically for cancer prevention due to potential side effects.
High-Risk Population Strategies
Individuals with elevated risk due to family history or genetic conditions may benefit from enhanced surveillance and prevention strategies.
Genetic counseling can help identify inherited cancer syndromes and guide appropriate screening and prevention approaches. Consider genetic testing if you have strong family histories of colorectal or related cancers.
Enhanced screening protocols may include earlier initiation of screening, more frequent examinations, or additional imaging studies.
Work with your healthcare provider to develop an appropriate screening schedule based on your individual risk profile.
For individuals with very high genetic risk, prophylactic surgical options may be considered. These decisions require careful consultation with specialized healthcare teams and consideration of individual circumstances.
Key Lifestyle Modifications
- Exercise regularly and maintain a healthy weight
- Avoid tobacco and limit alcohol consumption
Nutrition During Treatment
If you’re currently undergoing treatment for colorectal cancer, nutritional needs change significantly. Focus on maintaining adequate caloric intake and protein consumption to support healing and treatment tolerance.
Work with registered dietitians who specialize in oncology nutrition to develop personalized meal plans that address treatment-related side effects while supporting recovery.
Stay hydrated throughout treatment, as some therapies can affect the colon’s ability to absorb water efficiently. Consider electrolyte replacement if experiencing significant fluid losses.
Comprehensive FAQ Section
What age should I start getting screened for colorectal cancer?
Current guidelines recommend beginning colorectal cancer screening at age 45 for individuals at average risk, with screening continuing until age 75.
Those with elevated risk factors may need to start screening earlier, sometimes as young as age 40 or even earlier depending on specific risk factors.
How often do I need to get a colonoscopy?
For individuals at average risk with normal colonoscopy results, screening should occur every 10 years.
However, if polyps are found during the examination, your doctor may recommend more frequent screening, typically every 3-5 years depending on the number, size, and type of polyps discovered.
Are home stool tests as effective as colonoscopy for screening?
Home stool tests are effective screening tools when used appropriately, but they’re not as comprehensive as colonoscopy.
Stool tests can detect many cancers and some polyps, but they may miss smaller polyps or cancers that don’t bleed.
The advantage is their convenience and non-invasive nature, making them suitable for people who might otherwise avoid screening.
Can I prevent colorectal cancer through diet alone?
While diet plays a crucial role in colorectal cancer prevention, it cannot guarantee prevention on its own. A healthy diet should be combined with regular screening, physical activity, weight management, and avoidance of tobacco and excessive alcohol for optimal protection.
What symptoms should prompt me to see a doctor immediately?
Warning signs that warrant immediate medical attention include persistent changes in bowel habits, blood in stool, unexplained abdominal pain, unintentional weight loss, persistent fatigue, or iron deficiency anemia.
However, many colorectal cancers develop without symptoms, which is why regular screening is so important.
Is colorectal cancer hereditary?
While most colorectal cancers are not directly inherited, family history significantly influences risk.
Having a first-degree relative with colorectal cancer doubles your risk. Additionally, specific inherited genetic syndromes like Lynch syndrome or familial adenomatous polyposis substantially increase risk and require specialized management.
How much does obesity increase my risk of colorectal cancer?
Obesity, particularly excess abdominal weight, significantly increases colorectal cancer risk. Studies suggest that obesity can increase risk by 30-70% compared to individuals with healthy body weight. The good news is that weight loss can help reduce this risk.
Are there any foods that directly cause colorectal cancer?
While no single food directly causes cancer, processed meats are classified as Group 1 carcinogens by the World Health Organization, meaning there’s sufficient evidence they cause colorectal cancer.
Red meat is classified as a probable carcinogen. However, cancer development typically results from multiple factors rather than single dietary choices.
Can probiotics help prevent colorectal cancer?
Research on probiotics and colorectal cancer prevention is ongoing, with some promising early results.
Probiotics may help maintain healthy gut bacteria and reduce inflammation, potentially lowering cancer risk. However, more research is needed before probiotics can be definitively recommended for cancer prevention.
What’s the difference between colon cancer and rectal cancer?
Colon cancer develops in the large intestine (colon), while rectal cancer develops in the last several inches of the large intestine (rectum).
They’re often grouped together as colorectal cancer because they share many similarities in risk factors, prevention strategies, and treatment approaches.
How effective is colorectal cancer screening at preventing death?
Colorectal cancer screening is highly effective at reducing death rates. Regular screening can reduce colorectal cancer mortality by up to 60-70%.
This effectiveness comes from both early detection of existing cancers and prevention through removal of precancerous polyps.
Should I be concerned about radiation exposure from screening tests?
Most colorectal cancer screening tests don’t involve radiation exposure. Colonoscopy, sigmoidoscopy, and stool tests don’t use radiation.
CT colonography (virtual colonoscopy) does involve radiation, but the benefits of screening generally outweigh the minimal radiation risks for appropriate candidates.
Can stress increase my risk of colorectal cancer?
While chronic stress may contribute to various health problems and could potentially influence cancer risk through effects on immune function and inflammation, direct links between stress and colorectal cancer aren’t well established.
However, stress management remains important for overall health and may help you maintain other healthy behaviors.
What role does family history play in screening recommendations?
Family history significantly influences screening recommendations.
If you have a first-degree relative who developed colorectal cancer before age 60, or multiple relatives with the disease, you may need to start screening 10 years earlier than the age at which your relative was diagnosed, or by age 40, whichever comes first.
Are there any medications I should avoid that might increase my risk?
Some medications may slightly influence colorectal cancer risk, but the benefits of necessary medications typically outweigh potential risks.
Discuss any concerns about your medications with your healthcare provider, but don’t stop prescribed medications without medical guidance.
Taking Control of Your Colorectal Health
Protecting your colorectal health requires a proactive, multifaceted approach that combines regular screening with healthy lifestyle choices.
The encouraging news is that colorectal cancer is largely preventable through actions within your control.
Begin by scheduling appropriate screening based on your age and risk factors. This single step represents your most powerful tool for prevention and early detection.
Combine screening with dietary strategies that emphasize fiber-rich foods while limiting processed and red meats.
Incorporate regular physical activity into your routine, maintain a healthy body weight, and avoid tobacco products. If you drink alcohol, do so in moderation or consider eliminating it entirely for optimal protection.
Remember that small, consistent changes often produce more sustainable results than dramatic lifestyle overhauls. Start with one or two modifications and gradually build upon your successes.
Work with your healthcare provider to develop a personalized prevention plan that addresses your individual risk factors and health goals.
Action Steps for Immediate Implementation
- Schedule your screening appointment if you’re 45 or older
- Replace processed foods with whole grains and vegetables
- Incorporate 30 minutes of daily physical activity
Your colorectal health is largely within your control. By implementing these evidence-based strategies and maintaining regular medical care, you can significantly reduce your risk of developing colorectal cancer while promoting overall digestive health and well-being.

