The anterior cruciate ligament (ACL) is a vital component of knee stability, particularly during activities that involve pivoting, sudden stops, or directional changes.
When this ligament tears, it can significantly impact mobility and quality of life.
This guide provides detailed information about ACL injuries, reconstruction surgery options in Singapore, recovery expectations, and everything you need to know before undergoing this procedure.
Understanding the Knee and ACL
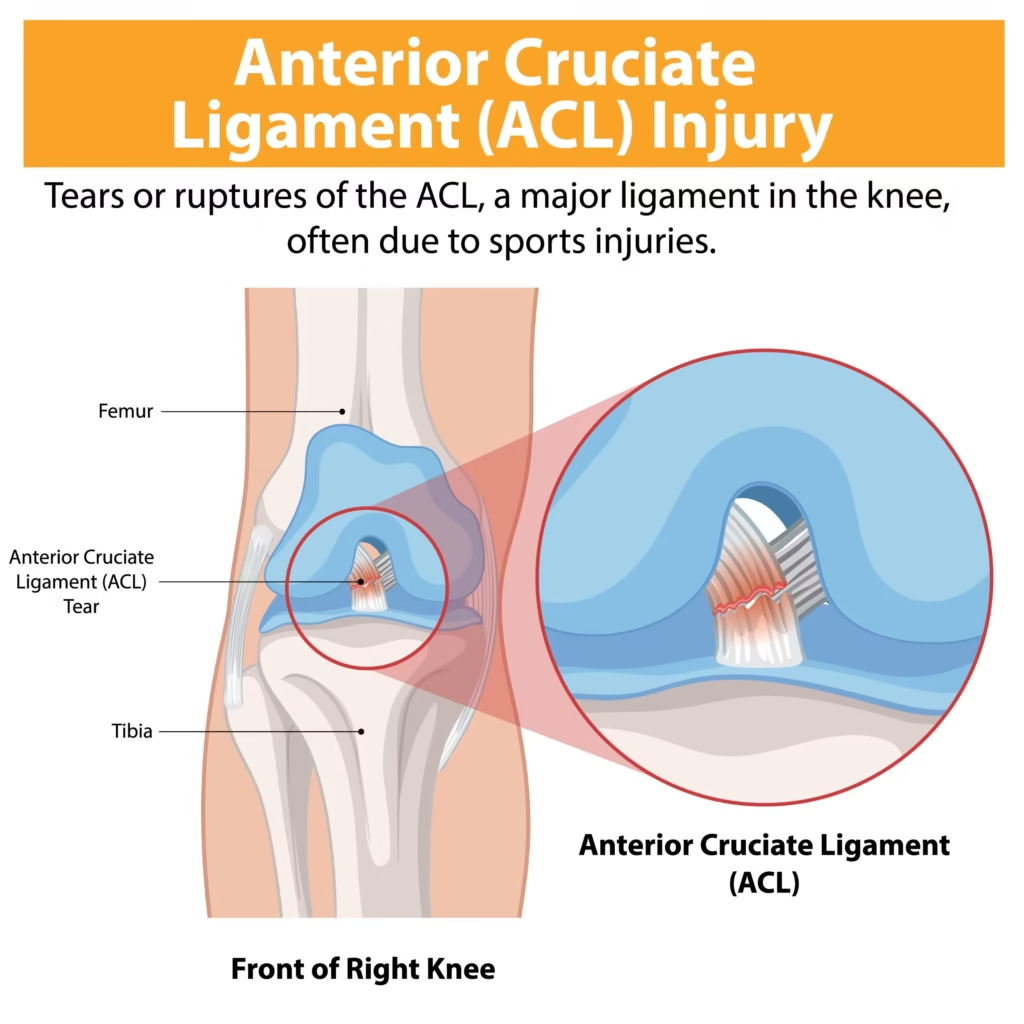
The knee is a complex joint connecting the thigh with the lower leg. It allows for flexion, extension, and limited rotation in certain positions.
Among the crucial stabilizing structures in the knee are the cruciate ligaments – the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL).
These ligaments are situated in the middle of the knee joint, connecting the femur (thigh bone) to the tibia (shin bone).
The ACL provides essential stability during movements that involve twisting or pivoting, serving as a critical component of knee joint mechanics.
Its primary functions include preventing excessive forward movement of the tibia relative to the femur, which maintains proper bone alignment during weight-bearing activities.
The ligament also limits rotational movements of the knee, preventing dangerous twisting motions that could damage other structures.
Additionally, the ACL provides overall stability during directional changes, allowing athletes and active individuals to perform cutting maneuvers and rapid direction changes safely.
Read more: Which Orthopedic Doctor in Singapore Should You Consider?
Common Causes of ACL Injuries
ACL injuries frequently occur during high-intensity sports and activities that place significant stress on the knee joint.
These injuries typically result from sudden stops or changes in direction, particularly when the movement is unexpected or uncontrolled.
Pivoting movements with the foot firmly planted create substantial rotational stress on the ACL, often leading to tears when the force exceeds the ligament’s capacity.
Direct blows or collisions to the knee, whether from contact with other players or objects, can cause immediate ACL damage.
Landing incorrectly from jumps, especially when the knee is in an awkward position or when the landing surface is uneven, frequently results in ACL injuries.
Falls that place extreme force on the knee joint, particularly those involving hyperextension or severe twisting, can also cause ligament tears.
Sports with higher ACL injury rates include football, basketball, volleyball, skiing, and other activities requiring rapid directional changes, with female athletes showing statistically higher injury rates in certain sports due to biomechanical and hormonal factors.
You might be interested: Knee Pain in Singapore: Causes, Treatment & Prevention
Recognizing ACL Injuries
When an ACL tear occurs, several distinct symptoms typically appear immediately or within hours of the injury.
Patients often report hearing or feeling a distinctive “popping” sound or sensation at the moment of injury, which is frequently accompanied by immediate awareness that something serious has occurred.
Rapid swelling of the knee joint usually develops within 24 hours as the body responds to the tissue damage and internal bleeding.
Significant pain, especially during movement or attempts to bear weight, is common and may worsen when trying to pivot or change direction.
One of the most characteristic symptoms is instability when walking or changing direction, with patients describing a feeling of the knee “giving way” or being unreliable during movement.
Limited range of motion develops as swelling increases and pain intensifies, making it difficult to fully bend or straighten the knee.
Many patients experience difficulty bearing weight on the affected leg, often requiring assistance to walk or completely avoiding weight-bearing activities.
Tenderness along the joint line is typically present and may be accompanied by visible bruising around the knee area.
If you experience these symptoms following a knee injury, seeking prompt medical evaluation is crucial for proper diagnosis and treatment planning, as early intervention can significantly impact recovery outcomes.
Related article: Best Orthopedic Doctor in JB for Singaporeans
Diagnosing ACL Tears
Proper diagnosis of an ACL injury involves a comprehensive evaluation that begins with a thorough physical examination to check knee stability using specific tests like the Lachman test and anterior drawer test.
Healthcare providers conduct a detailed review of how the injury occurred, including the mechanism of injury, the position of the knee at impact, and any immediate symptoms experienced.
An MRI scan is typically performed to confirm the diagnosis definitively and identify any associated injuries such as meniscus tears, cartilage damage, or injuries to other ligaments.
Sometimes, X-rays are necessary to rule out fractures or bone injuries that may have occurred simultaneously with the ACL tear.
Early and accurate diagnosis helps determine the most appropriate treatment approach and timeline, allowing for optimal planning of both surgical and non-surgical interventions.
You might like: Arthritis Treatment in Singapore: Causes, Risks, Symptoms
Treatment Options for ACL Injuries
Non-Surgical Management
Not all ACL injuries require surgical intervention, and non-surgical approaches may be suitable for specific patient populations.
These conservative treatments are often appropriate for individuals with partial tears who demonstrate good knee stability during clinical testing.
Less active people who don’t participate in pivoting sports or high-demand activities may achieve satisfactory outcomes without surgery.
Elderly patients with lower physical demands and those who are willing to modify their activity levels may also benefit from non-surgical management.
Non-surgical treatment typically includes comprehensive physical therapy programs designed to strengthen surrounding muscles, particularly the quadriceps and hamstrings, which can help compensate for ACL deficiency.
Specialized bracing provides additional support during activities and may help prevent episodes of instability.
Activity modification involves avoiding high-risk movements such as pivoting, cutting, and jumping sports while allowing participation in lower-risk activities.
Anti-inflammatory medications are used to manage pain and swelling during the acute phase and throughout the rehabilitation process.
Read more: Sports Doctors in Singapore: Guide to Finding a Suitable Specialist
Surgical Treatment: ACL Reconstruction
ACL reconstruction becomes necessary when conservative treatment is insufficient to restore adequate knee function and stability.
Surgery is typically recommended when the tear is complete or severe, resulting in significant functional impairment.
Patients who exhibit significant knee instability during daily activities or clinical testing are strong candidates for surgical intervention.
Those who wish to return to pivoting sports or physically demanding activities that require reliable knee stability almost always require surgical reconstruction to safely resume their desired activity level.
The presence of associated injuries to other knee structures, such as meniscus tears or collateral ligament damage, often necessitates surgical treatment to address all injured components comprehensively.
Additionally, when conservative treatment has been attempted for an appropriate period but has not provided adequate improvement in symptoms or function, ACL reconstruction may be the most effective option for restoring knee stability and preventing long-term complications such as secondary meniscus tears or early-onset arthritis.
You might like: Total Knee Replacement Surgery in Singapore
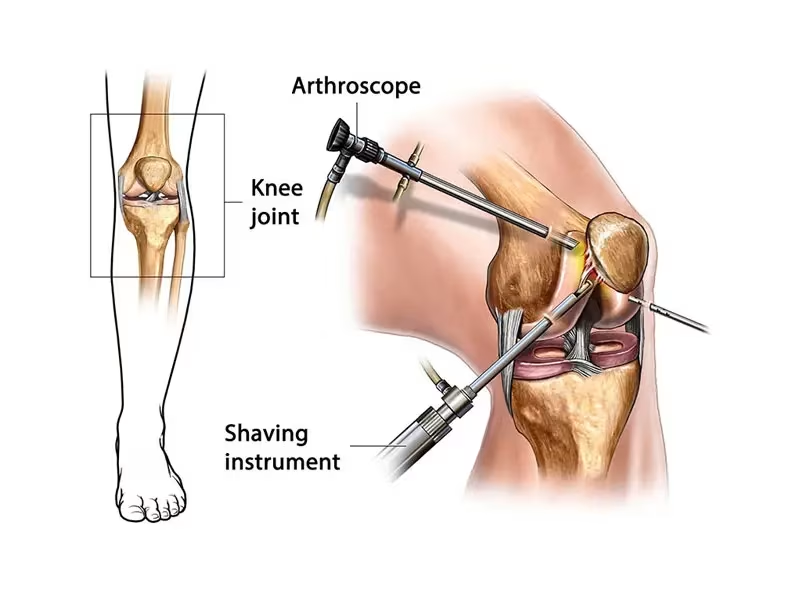
What is ACL Reconstruction Surgery?
ACL reconstruction is a surgical procedure that replaces the torn ligament with a graft tissue.
Unlike simple repairs, reconstruction involves removing the damaged ligament and replacing it with a healthy tissue graft to restore knee stability and function.
The procedure is typically performed arthroscopically (minimally invasive technique) using small incisions and specialized instruments, including a tiny camera (arthroscope) to visualize the inside of the joint.
You might like: Hip Replacement Surgery in Singapore: Cost, Risks
Graft Options for ACL Reconstruction
Several graft options are available for ACL reconstruction:
Autografts (from your own body):
- Hamstring tendon graft: Currently the most popular option worldwide, using portions of the hamstring tendons
- Bone-patellar tendon-bone graft: Involves taking the middle third of the patellar tendon with bone plugs from the kneecap and tibia
- Quadriceps tendon graft: Uses a portion of the quadriceps tendon above the kneecap
Allografts (from a donor):
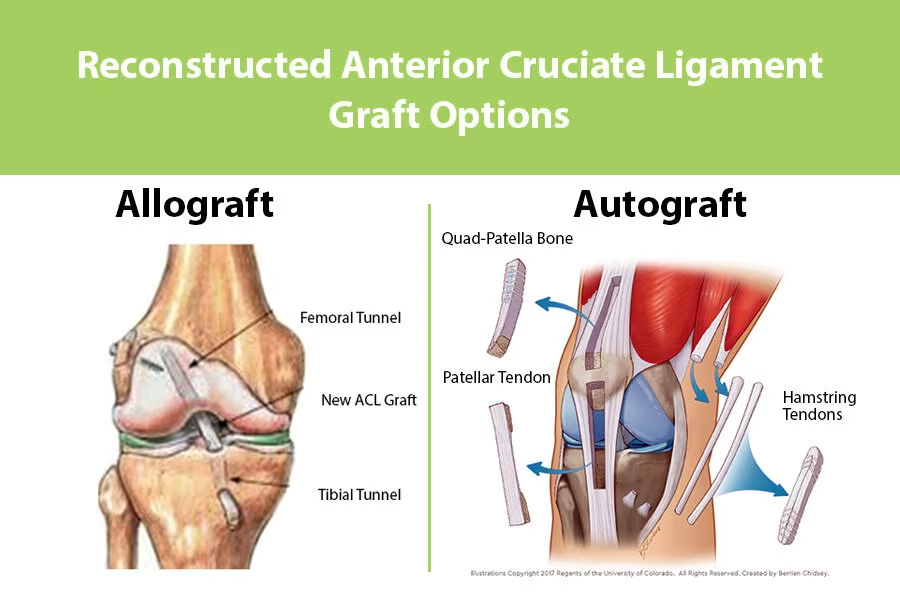
- Tendon grafts from deceased donors
- Often used for revision surgeries or in older patients
The choice of graft depends on various factors, including:
- Patient age and activity level
- Surgeon’s preference and expertise
- Desired recovery timeline
- Previous surgeries or injuries
- Individual anatomical considerations
Preparing for ACL Reconstruction Surgery
Pre-surgery Assessment
Before undergoing ACL reconstruction surgery, patients will undergo a comprehensive evaluation process to ensure optimal surgical outcomes.
This includes a thorough physical examination to assess knee stability, range of motion, and overall joint health.
Healthcare providers will conduct a detailed review of medical history, including previous injuries, medications, allergies, and any underlying health conditions that might affect surgery or recovery.
Imaging tests such as MRI scans and X-rays are essential components of the pre-surgical assessment, providing detailed views of the torn ACL and any associated injuries to cartilage, meniscus, or other ligaments. In some cases, patients may be recommended for “prehabilitation,” a specialized pre-surgery rehabilitation program designed to strengthen the knee and surrounding muscles, which can significantly improve post-operative outcomes and accelerate the recovery process.
Days Before Surgery
Proper preparation in the days leading up to surgery is crucial for optimal results and reduced complications.
Patients must avoid smoking for at least one week before surgery, as smoking can significantly impede recovery by reducing blood flow and oxygen delivery to healing tissues.
It is essential to stop eating and drinking after midnight the night before surgery to ensure an empty stomach for safe anesthesia administration.
Patients should carefully follow any specific medication instructions provided by their surgeon, which may include temporarily discontinuing certain medications or starting prescribed pre-operative medications.
Taking a shower with antiseptic wash both the evening before and the morning of surgery helps reduce the risk of surgical site infections.
Additionally, arranging for reliable transportation to and from the hospital and securing assistance during the initial recovery period is essential, as patients will not be able to drive immediately following surgery.
The ACL Reconstruction Procedure
ACL reconstruction in Singapore is typically performed under general anesthesia and takes approximately 90 minutes. The general steps include:
- Anesthesia administration: You’ll be placed under general anesthesia to ensure you’re comfortable and pain-free
- Arthroscopic examination: Small incisions allow insertion of the arthroscope to assess the damage
- Graft harvesting: If using an autograft, the surgeon will harvest the chosen tendon graft
- Damaged ACL removal: The torn ligament is removed
- Tunnel creation: Tunnels are drilled in the femur and tibia at precise positions
- Graft placement: The graft is pulled through the tunnels and positioned where the original ACL was located
- Graft fixation: Specialized screws or other fixation devices secure the graft in place
- Final assessment: The knee is examined for proper graft tension and placement
- Closure: The small incisions are closed with stitches or surgical tape
- Dressing and bracing: A sterile dressing is applied, and the knee is placed in a protective brace
Cost of ACL Reconstruction in Singapore
According to Ministry of Health data, the estimated bill range for ACL reconstruction surgery in a private hospital in Singapore is approximately $26,519 to $33,204, based on 2021 data.
However, the exact cost can vary significantly depending on several factors that patients should consider when planning for surgery.
These cost variables include whether the procedure is performed in a public or private hospital, with private facilities typically charging higher fees for enhanced amenities and shorter waiting times.
Surgeon’s fees vary based on experience, reputation, and the complexity of the case. The type of graft used, whether it’s taken from the patient’s own tissue (autograft) or from a donor (allograft), can also affect the overall cost.
The length of hospital stay, which typically ranges from one to three days, influences the final bill, as does the need for any additional procedures if complications arise or other injuries are discovered during surgery.
Fortunately, ACL reconstruction surgery is typically insurance-claimable and Medisave-approved in Singapore, making it more accessible to patients who need this important procedure.
It is advisable to check with your insurance provider regarding specific coverage details and any pre-authorization requirements before scheduling surgery.
Post-Surgery Recovery and Care
Immediate Post-operative Period (Days 1-3)
The immediate post-operative period requires careful monitoring and pain management in a controlled hospital environment.
Hospital stays typically last 2-3 days, during which medical staff monitor for complications and ensure proper wound healing begins.
Pain management with prescribed medications is essential for patient comfort and allows for early mobilization, which is crucial for preventing complications such as blood clots.
Initial physical therapy exercises begin within hours of surgery, focusing on gentle range-of-motion movements and basic muscle activation.
Patients are fitted with a knee brace and taught proper elevation techniques to control swelling and promote circulation. Ice application through cryotherapy helps reduce inflammation and provides additional pain relief.
During this period, patients learn to use crutches safely for mobility while protecting the surgical site and newly reconstructed ligament.
Early Recovery Phase (Weeks 1-6)
The early recovery phase focuses on protecting the healing graft while gradually restoring basic function.
Patients continue crutch walking with progressive weight-bearing as directed by their surgeon, typically starting with partial weight-bearing and advancing to full weight-bearing as healing progresses.
Regular wound care is essential, requiring patients to keep dressings clean and dry while monitoring for signs of infection such as increased redness, warmth, or drainage.
Prescribed physical therapy exercises become more structured and frequent, focusing on maintaining range of motion and preventing muscle atrophy.
Knee brace usage continues according to the surgeon’s specific instructions, often worn during all weight-bearing activities for the first several weeks.
Pain and swelling management remains important, with patients using prescribed medications, ice, and elevation as needed.
Regular follow-up appointments allow healthcare providers to monitor healing progress and adjust treatment plans as necessary.
Intermediate Recovery Phase (Weeks 6-12)
During the intermediate recovery phase, patients experience significant improvements in function and begin more active rehabilitation.
There is progressive reduction in brace usage as the knee demonstrates improved stability and the graft continues to heal and integrate.
The intensity of strengthening exercises increases substantially, with focus shifting toward rebuilding muscle strength and endurance that was lost during the initial recovery period.
Improving range of motion becomes a primary goal, with patients working to regain full knee flexion and extension through dedicated stretching and mobilization exercises.
There is gradual return to normal walking patterns as strength and confidence improve, with most patients able to walk without assistive devices by the end of this phase.
Special focus is placed on rebuilding quadriceps and hamstring strength, as these muscle groups are essential for knee stability and function.
Advanced Recovery Phase (Months 3-6)
The advanced recovery phase marks the transition from basic rehabilitation to more demanding functional training.
Patients begin functional exercises including running and jumping, initially under close supervision to ensure proper form and technique. More challenging balance and coordination training helps restore proprioception, which is the body’s ability to sense joint position and movement.
The introduction of sport-specific movements begins gradually, with exercises tailored to the individual’s intended return-to-activity goals.
Agility training and plyometrics (explosive movement exercises) are progressively incorporated to prepare the knee for the demands of athletic activities.
Continued strength building remains a priority, with emphasis on achieving strength levels that meet or exceed pre-injury levels.
Return to Sports Phase (Months 6-12)
The final phase of recovery focuses on safe return to full athletic participation through comprehensive sport-specific rehabilitation.
This phase involves detailed assessment of knee function, strength, and stability to ensure readiness for sports participation.
Gradual reintroduction to sports activities follows a carefully planned progression, starting with low-intensity, controlled movements and advancing to full-speed, competitive activities.
Testing and assessment of knee function and stability are performed regularly using objective measures such as hop tests, strength assessments, and movement analysis.
Throughout this phase, preventive exercises designed to reduce re-injury risk are emphasized, including proper warm-up routines, neuromuscular training, and techniques for safe landing and cutting movements.
The ultimate goal is not just to return to sports, but to do so with reduced risk of future ACL injuries.
Return to Sports Timeline
The timeline for returning to various activities after ACL reconstruction:
- Low-impact activities (swimming, cycling): 2-3 months
- Running on flat surfaces: 4-5 months
- Cutting and pivoting movements: 6-9 months
- Full return to contact/pivoting sports: 9-12 months
It’s crucial not to rush the return to sports, particularly during months 4-8 when the graft is undergoing remodeling and may be at its weakest. Following your surgeon’s and physiotherapist’s guidance is essential for a successful return to sports.
Rehabilitation Process After ACL Reconstruction
Rehabilitation is a critical component of successful ACL reconstruction outcomes. The general timeline includes:
Weeks 1-2
- Regular icing and elevation to reduce knee swelling
- Protected weight-bearing with crutches
- Passive range of motion exercises
- Initial quadriceps, hamstring, and calf strengthening
Weeks 3-4
- Progression to walking with one crutch
- Expanded range of motion exercises
- Continued strengthening of supporting muscles
Weeks 5-6
- Gradual reduction in brace usage
- Increased intensity of muscle strengthening
- More general knee movement exercises
Week 10
- Dynamic movement training in multiple directions
- Introduction of isokinetic exercises
Month 3
- Functional exercises like running and jumping
- Introduction of directional changes as coordination improves
Months 4-5
- Focus on maximizing endurance and strength
- Advanced neuromuscular control exercises
- Acceleration/deceleration training with directional variations
Potential Complications and Risk Factors
While ACL reconstruction is generally safe and effective, potential complications include:
Graft Failure or Re-rupture
Risk factors include:
- Early return to pivoting sports
- Age under 20 years
- Using allograft tissue (approximately 5 times higher risk than autografts)
- Poor rehabilitation compliance
Infection
Though rare, infection prevention measures include:
- Pre-operative antiseptic washes
- Prophylactic antibiotics
- Sterile surgical techniques
- Proper wound care
Persistent Pain or Stiffness
May result from:
- Inadequate rehabilitation
- Arthrofibrosis (excessive scar tissue)
- Improper graft placement or tension
Muscle Weakness
Often preventable through:
- Early and consistent rehabilitation
- Progressive strengthening exercises
- Proper gait training
Am I a Candidate for ACL Reconstruction?
You may be a suitable candidate for ACL reconstruction if you:
- Have a complete ACL tear with knee instability
- Are physically active and wish to return to sports or demanding activities
- Experience persistent knee pain and difficulty with movements despite conservative treatments
- Are relatively young (though age is not a strict limitation)
- Have additional knee injuries, such as meniscus or cartilage damage
Conversely, you might consider non-surgical options if you:
- Have a partial tear with good knee stability
- Participate primarily in straight-line activities (walking, swimming, cycling)
- Have lower activity goals or demands
- Have severe osteoarthritis or other knee degeneration
Preventing ACL Injuries
Several strategies can help reduce the risk of ACL injuries:
- Proper strength training: Focus on core, hip, and leg strength
- Neuromuscular training: Programs that improve landing mechanics and body control
- Appropriate warm-up: Dynamic stretching before activities
- Proper footwear: Suitable shoes for your sport and surface
- Technique improvement: Learning proper jumping, landing, and cutting techniques
- Adequate rest: Avoiding overtraining and fatigue
Frequently Asked Questions
Can a torn ACL heal by itself?
A complete ACL tear cannot heal by itself. The ACL has poor blood supply, which limits its natural healing capacity.
While symptoms may improve with time and rehabilitation, the structural stability provided by an intact ACL cannot be naturally restored once completely torn.
Non-surgical treatments may help manage symptoms, but they cannot fully restore the knee’s stability. Surgery is typically necessary for individuals wanting to return to pivoting sports or activities.
What is the best time to undergo ACL surgery after injury?
The optimal timing for ACL reconstruction is typically within a few weeks to a few months following the injury. This allows time for the initial swelling to subside and for some pre-surgery rehabilitation to improve range of motion and strength.
Research suggests that delaying surgery beyond 12 weeks may increase the risk of additional knee damage and potentially reduce the likelihood of optimal outcomes.
However, the exact timing depends on individual factors including overall health, extent of injury, and lifestyle considerations.
How long does recovery take after ACL reconstruction?
Full recovery after ACL reconstruction typically takes 9-12 months, though this varies based on individual factors.
The general timeline includes: initial recovery and pain management (1-2 weeks), early rehabilitation focusing on range of motion and basic strengthening (2-6 weeks), progressive strengthening (6-12 weeks), and advanced rehabilitation with return to sports training (3-12 months).
Most patients can resume daily activities within 1-3 months, light recreational activities by 4-6 months, and competitive sports between 9-12 months, following clearance from their surgeon.
Will I need crutches after ACL surgery?
Yes, crutches are necessary after ACL surgery. Most patients require crutches for approximately 2-4 weeks post-surgery, depending on individual recovery progress and surgeon preferences.
Initially, you’ll likely be instructed to minimize weight-bearing on the operated leg. As your strength and stability improve, your physiotherapist will guide you through progressive weight-bearing and eventually transition you away from crutches.
Proper crutch technique is important to avoid developing compensatory movement patterns that could hinder your recovery.
Can I prevent re-injury after ACL reconstruction?
Yes, several strategies can help reduce the risk of re-injury after ACL reconstruction.
These include: completing the full rehabilitation program (9-12 months), maintaining ongoing strength and conditioning exercises, using proper technique during sports and physical activities, wearing appropriate footwear, using preventive bracing during high-risk activities if recommended, and avoiding return to competitive sports until cleared by your surgeon and physiotherapist.
Research shows that proper completion of rehabilitation and neuromuscular training can significantly reduce re-injury rates.
How do I choose between hamstring and patellar tendon grafts?
The choice between hamstring and patellar tendon grafts depends on several factors.
Hamstring grafts typically result in less post-operative pain, smaller incisions, and lower risk of anterior knee pain, making them popular for general population and recreational athletes.
Patellar tendon grafts may offer slightly faster incorporation and stronger initial fixation, potentially beneficial for high-level athletes requiring early return to sport.
Your surgeon will consider your activity goals, occupation, previous injuries, and anatomical factors when recommending the most suitable graft for your specific situation.
Can I undergo ACL reconstruction if I’m over 40?
Yes, ACL reconstruction can be appropriate for patients over 40, though considerations differ from younger patients.
The decision should factor in your activity level, lifestyle goals, knee stability, and presence of other conditions like arthritis.
Many active adults over 40 achieve excellent results with ACL reconstruction when they wish to maintain an active lifestyle involving pivoting sports or physically demanding activities.
Your surgeon will consider your specific circumstances, potentially modifying surgical techniques or rehabilitation protocols to optimize outcomes for your age group.
How much does physiotherapy cost after ACL surgery in Singapore?
Physiotherapy costs after ACL surgery in Singapore typically range from $80-$150 per session.
Most patients require approximately 20-30 sessions over 6-9 months, bringing the total physiotherapy cost to roughly $1,600-$4,500.
These costs may be partially covered by insurance or Medisave, depending on your specific coverage plan.
Given the critical importance of rehabilitation to successful outcomes, this represents an essential investment in your recovery process.
Check with your insurance provider regarding specific coverage details for post-surgical rehabilitation.
Can I drive after ACL surgery?
Driving after ACL surgery depends on which knee was operated on and your recovery progress.
For right knee surgery, most patients can resume driving after 4-6 weeks, once they’ve discontinued narcotic pain medications and can safely operate the brake pedal.
For left knee surgery (in automatic transmission vehicles), driving may be possible sooner, typically around 2-3 weeks.
However, your surgeon will provide specific guidance based on your individual recovery, and you should only resume driving when you can react quickly in emergency situations without pain or limitation.
What happens if I delay ACL surgery?
Delaying ACL surgery may lead to several potential consequences.
These include increased risk of meniscal tears and cartilage damage due to ongoing knee instability, development of early osteoarthritis, chronic pain and instability affecting daily activities, muscle atrophy and weakness, and potentially more complicated surgical repair when eventually performed.
Research indicates that reconstruction performed within 3 months of injury tends to yield better outcomes than significantly delayed procedures.
However, individual circumstances vary, and your orthopedic surgeon can help assess the specific risks associated with delaying surgery in your case.
By understanding the full scope of ACL reconstruction—from injury to recovery—patients in Singapore can make informed decisions about their treatment options and approach rehabilitation with realistic expectations.
Remember that successful outcomes depend not only on skilled surgical technique but also on dedicated rehabilitation and adherence to recovery protocols.

