Frozen shoulder, medically known as adhesive capsulitis, is a condition characterized by stiffness, pain, and limited range of motion in the shoulder joint.
This debilitating condition can significantly impact daily activities, making simple tasks like reaching for objects, getting dressed, or combing hair extremely challenging.
In this comprehensive guide, we’ll explore the causes, symptoms, stages, diagnosis, and treatment options available in Singapore for individuals suffering from frozen shoulder.
Read more: Which Orthopedic Doctor in Singapore Should You Consider?
What is Frozen Shoulder?
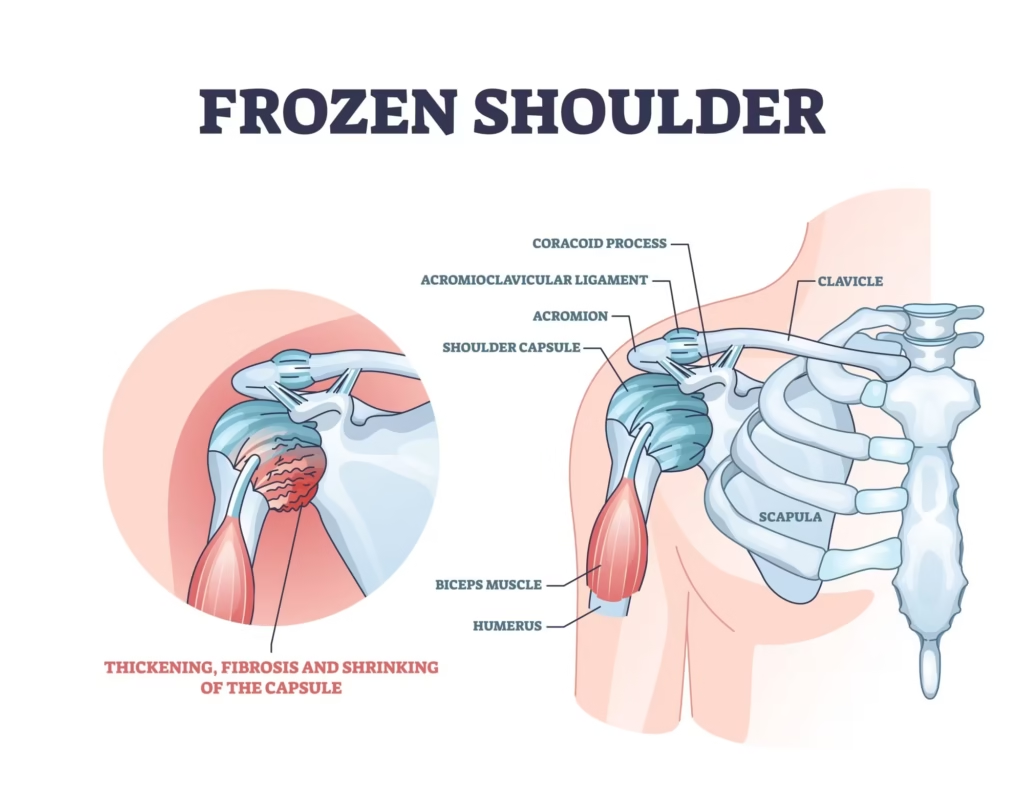
Frozen shoulder occurs when the shoulder capsule (the connective tissue surrounding the shoulder joint) becomes inflamed, thickened, and contracted.
This inflammation reduces the actual space inside the joint, limiting the shoulder’s ability to move in various directions. The condition most commonly affects adults between the ages of 40 and 60, with women being more susceptible than men.
Related article: ACL Reconstruction Surgery in Singapore: Causes, Costs
Stages of Frozen Shoulder
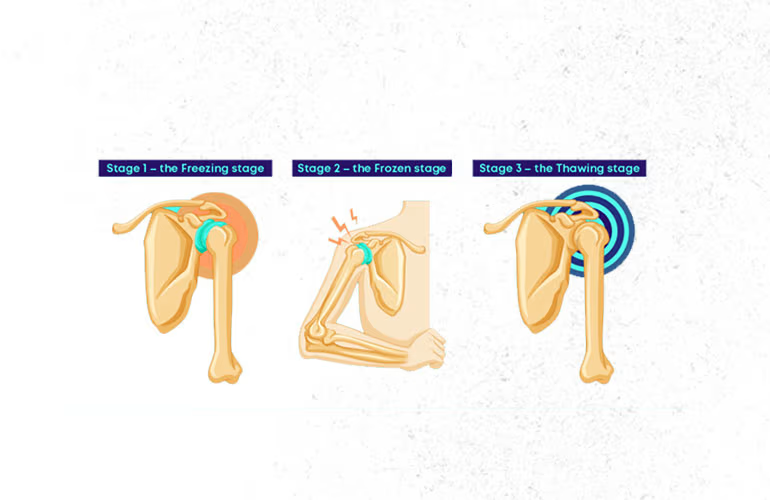
Frozen shoulder typically progresses through three distinct stages, each with its own characteristics:
Stage 1: Freezing Stage (6-12 weeks)
This stage is characterized by a gradual onset of shoulder pain that worsens with movement and is often worse at night.
During this period, shoulder movement becomes increasingly limited as pain intensifies.
This painful stage can last from 6 weeks up to 9 months, making it the most uncomfortable phase for patients.
Stage 2: Frozen Stage (4-6 months)
During the frozen stage, pain may begin to diminish, but stiffness remains or actually worsens significantly.
Patients experience significant restriction in shoulder movement, which makes daily activities increasingly difficult due to limited mobility.
This stage generally lasts between 4 to 9 months and represents the period of maximum stiffness.
Related article: Shoulder Pain in Singapore: Causes, Treatments, Recovery
Stage 3: Thawing Stage (6-24 months)
The thawing stage brings gradual improvement in shoulder movement as pain continues to decrease progressively.
Shoulder motion slowly returns toward normal function, though complete recovery may take anywhere from 6 months to 2 years, requiring patience and consistent treatment throughout this extended period.
Causes and Risk Factors of Frozen Shoulder
The exact cause of frozen shoulder isn’t always clear, but medical professionals can classify it into two main categories based on underlying factors.
Primary Frozen Shoulder
Primary frozen shoulder occurs without an obvious identifiable cause, also known as idiopathic frozen shoulder.
Currently, no comprehensive etiological model exists to fully explain why this condition develops spontaneously, though it is associated with certain risk factors that may predispose individuals to developing the condition.
You might like: Arthritis Treatment in Singapore: Causes, Risks, Symptoms
Secondary Frozen Shoulder
Secondary frozen shoulder develops following an identifiable cause and is often related to injury, surgery, or prolonged immobilization of the shoulder joint.
This type shows clear evidence of trauma that directly affects the shoulder joint, with common examples including rotator cuff tears, fractures, or post-surgical complications that trigger the inflammatory response leading to adhesive capsulitis.
Risk Factors
Several factors increase the likelihood of developing frozen shoulder:
- Age and Gender: More common in people over 40 years old, with women affected twice as often as men
- Diabetes: Diabetic patients have five times the risk compared to non-diabetics
- Other Medical Conditions: Thyroid disorders (both hyperthyroidism and hypothyroidism), cardiovascular disease, and Parkinson’s disease
- Immobility: Prolonged shoulder immobilization following injury or surgery
- Post-surgery: Especially after shoulder reconstruction or mastectomy procedures
This might help: Osteoarthritis Treatment in Singapore: Symptoms, Prevention
Signs and Symptoms of Frozen Shoulder
The primary symptoms of frozen shoulder include:
- Progressive decrease in shoulder joint mobility in all directions
- Pain that is typically dull or aching, often worse at night and during movement
- Difficulty with daily activities such as reaching across a table, putting on shirts or bras
- Pain when trying to sleep on the affected shoulder
- Limited motion on both passive and active movement
- “Grinding” sensation when moving the shoulder
Diagnosis of Frozen Shoulder
Diagnosing frozen shoulder typically involves:
Medical History Assessment
Your doctor will discuss your symptoms, pain patterns, and potential risk factors that may have contributed to developing the condition.
Physical Examination
The doctor will assess the range of motion in both shoulders, comparing the affected shoulder with the healthy one.
This involves checking for pain during movement and noting any movement limitations.
Imaging Tests
While not always necessary, imaging tests may be used to rule out other conditions:
- X-rays to rule out arthritis or structural abnormalities
- MRI scans to examine soft tissues and rule out rotator cuff tears
The diagnosis is usually clinical, based on the characteristic pattern of symptoms and physical examination findings.
You might be interested: Neck Pain in Singapore: Causes, Treatments, Prevention
Frozen Shoulder Treatment Options in Singapore
Treatment for frozen shoulder in Singapore focuses on alleviating pain, reducing inflammation, and restoring range of motion. The approach typically progresses from conservative methods to more invasive interventions if needed.
Non-Surgical Treatments
1. Medications
Over-the-counter pain relievers such as ibuprofen, aspirin, or acetaminophen are commonly used to reduce pain and inflammation in frozen shoulder patients.
For more severe cases, prescription anti-inflammatory medications may be necessary to provide adequate symptom control and improve patient comfort during the recovery process.
2. Corticosteroid Injections
Corticosteroid injections are administered directly into the shoulder joint to reduce inflammation and pain effectively.
These injections are particularly effective during the early stages of frozen shoulder and help improve mobility significantly.
However, repeated injections are discouraged as they may cause further damage to the joint structures over time.
Related article: Sports Doctors in Singapore: Guide to Finding a Suitable Specialist
3. Physiotherapy
Physiotherapy serves as a cornerstone of frozen shoulder treatment, involving a comprehensive approach to restore function and mobility.
Treatment includes stretching exercises designed to improve range of motion and prevent atrophy of surrounding shoulder muscles, along with trigger point massage techniques to release muscle tension.
Ultrasound and heat therapy are used to reduce inflammation and promote healing, while strengthening exercises help improve shoulder stability and function.
Regular, consistent therapy sessions are crucial for achieving optimal results and preventing long-term complications.
4. Hydrodilatation
Hydrodilatation involves the injection of saline solution into the contracted shoulder joint to break adhesions that limit movement.
This procedure helps increase shoulder joint volume and improve mobility effectively, and it may be combined with corticosteroid injection for enhanced therapeutic effect and faster symptom relief.
5. Heat and Cold Therapy
Applying ice packs helps reduce inflammation and pain during acute phases of the condition, while heat therapy helps improve blood circulation and relaxes tense muscles around the shoulder joint.
Both modalities can be used alternately throughout the day for optimal pain relief and to support the healing process.
6. Transcutaneous Electrical Nerve Stimulation (TENS)
TENS therapy uses mild electrical current to help relieve pain by blocking nerve signals that transmit pain sensations to the brain.
This non-invasive approach provides a safe treatment option that can effectively complement other therapies without causing additional side effects or complications.
Surgical Treatments
If conservative treatments fail to provide sufficient relief after 6 months, surgical options may be considered:
1. Shoulder Arthroscopy (Keyhole Capsular Release)
- Minimally invasive procedure performed under general anesthesia
- Small incisions are made around the shoulder
- A tiny camera (arthroscope) guides the surgeon
- Specialized instruments are used to cut through scar tissue and release the tight joint capsule
- Relieves inflammation and promotes improved range of motion
- After surgery, continued physiotherapy is essential to maintain mobility gains
2. Manipulation Under Anesthesia (MUA)
- Performed under general anesthesia
- The surgeon manually moves the shoulder joint in various directions
- Helps break up adhesions and increase mobility
- No incisions are made during this procedure
- Often performed in conjunction with arthroscopic release
3. Capsular Release
- Surgical procedure to cut through tight portions of the joint capsule
- Can be performed arthroscopically or through traditional open surgery
- Particularly useful for severe cases with significant contracture
Recovery Timeline and Prognosis
The recovery timeline for frozen shoulder varies significantly depending on:
- Severity of the condition
- Treatment approach
- Patient adherence to the treatment plan
- Individual healing factors
About 90% of patients with frozen shoulder show improvement after six months of non-operative treatment. However, approximately 10% may require surgical intervention.
Full recovery can range from several months to 2-3 years. It’s important for patients to understand that recovery is often gradual and requires patience and commitment to the treatment plan.
Prevention Strategies for Frozen Shoulder
While it may not be possible to prevent frozen shoulder in every case, these strategies can help reduce risk:
- Regular Exercise: Maintain shoulder mobility and strength, particularly after injuries or surgeries
- Managing Chronic Conditions: Effectively control conditions like diabetes and thyroid disorders
- Early Intervention: Seek prompt treatment for shoulder pain or stiffness
- Regular Stretching: Incorporate shoulder stretching exercises into daily routines, especially for those at higher risk
When to Return to Normal Activities
Everyone recovers from frozen shoulder at different rates. Generally, you can consider returning to normal or vigorous activities when:
- Your affected shoulder has regained almost full range of motion without pain
- The strength in your affected shoulder is comparable to your unaffected shoulder
Frequently Asked Questions
What is the difference between adhesive capsulitis and pericapsulitis?
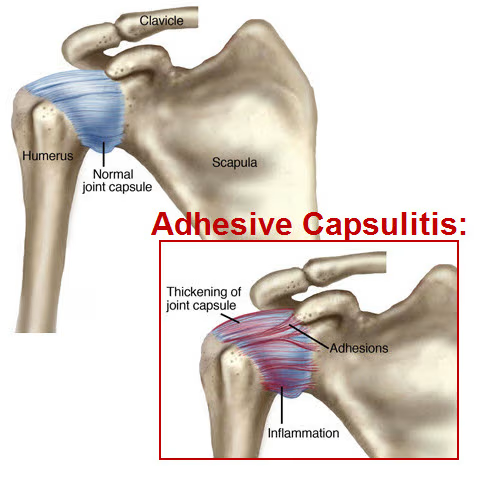
Adhesive capsulitis refers to the inflammation of the shoulder capsule that leads to tightening and adhesions forming within the joint capsule.
Pericapsulitis, on the other hand, refers to inflammation occurring around the shoulder joint, affecting surrounding tissues, muscles, and tendons.
Both terms are commonly used to describe frozen shoulder, with slightly different emphasis on where the inflammation occurs.
How long does it take for a frozen shoulder to recover completely?
The recovery timeline varies significantly between individuals. While some may experience improvement within 6-9 months, complete recovery can take anywhere from 1 to 3 years.
The condition typically progresses through the freezing, frozen, and thawing stages, with each stage lasting several months.
About 90% of patients see improvement with non-surgical treatments, while approximately 10% may require surgical intervention for full recovery.
Is frozen shoulder more common in people with certain medical conditions?
Yes, frozen shoulder occurs more frequently in people with certain medical conditions. Diabetic patients have five times the risk compared to non-diabetics.
Other conditions that increase risk include thyroid disorders (both hyperthyroidism and hypothyroidism), cardiovascular disease, and Parkinson’s disease.
The exact mechanism linking these conditions to frozen shoulder isn’t fully understood, but may involve changes in collagen formation and inflammatory responses.
What happens if frozen shoulder is left untreated?
If left untreated, frozen shoulder may eventually improve on its own, but the process can be extremely slow and painful, potentially taking up to 2-3 years.
During this time, patients may experience significant pain, severely restricted mobility, muscle atrophy, and reduced quality of life.
Additionally, compensatory movements to avoid shoulder pain can lead to other musculoskeletal issues. Early intervention typically results in faster recovery and better outcomes.
Can frozen shoulder come back after treatment?
While recurrence in the same shoulder is relatively uncommon (occurring in less than 5% of cases), having frozen shoulder in one shoulder increases the risk of developing it in the opposite shoulder by 20-30%.
Factors that may contribute to recurrence include incomplete treatment, failure to maintain mobility exercises after recovery, and underlying medical conditions like diabetes.
Proper management of risk factors and maintenance exercises can help prevent recurrence.
Are there any specific exercises recommended for frozen shoulder?
Specific exercises for frozen shoulder should be prescribed by a physiotherapist based on individual assessment and the stage of the condition.
Generally, gentle stretching exercises are recommended to maintain and improve range of motion. These may include pendulum exercises, wall crawls, cross-body reaches, and gentle rotation stretches.
The intensity and types of exercises will evolve as recovery progresses. It’s important not to push through significant pain, as this may exacerbate inflammation.
What is the role of diet in managing frozen shoulder?
While no specific diet has been proven to directly treat frozen shoulder, maintaining proper nutrition can support the healing process.
Anti-inflammatory foods such as fatty fish, berries, nuts, olive oil, and leafy greens may help reduce overall inflammation. Proper hydration is also important for joint health.
For patients with diabetes or other metabolic conditions that increase frozen shoulder risk, managing these conditions through diet can indirectly improve outcomes and reduce recurrence risk.
How do I know if my shoulder pain is frozen shoulder or something else?
Frozen shoulder has a characteristic pattern: gradual onset of pain, progressive stiffness, and limited range of motion in all directions (especially external rotation and abduction).
The condition typically affects people aged 40-60 and progresses through distinct stages. Other shoulder conditions like rotator cuff tears, arthritis, or bursitis may present differently.
A proper diagnosis from a healthcare professional is essential, as they can perform specific tests to differentiate frozen shoulder from other conditions.
What is the success rate of surgery for frozen shoulder?
The success rate for surgical interventions in frozen shoulder is generally high, with approximately 85-95% of patients experiencing significant improvement in pain and range of motion.
Arthroscopic capsular release combined with manipulation under anesthesia tends to show particularly good outcomes.
However, successful long-term results depend heavily on proper post-surgical rehabilitation and physiotherapy.
Without appropriate follow-up care, adhesions may reform, limiting the benefits of surgery.
Can I prevent frozen shoulder if I have diabetes?
While having diabetes increases the risk of developing frozen shoulder, there are preventive measures that can help.
Maintaining good glycemic control is essential, as high blood sugar levels can cause collagen to become sticky in shoulder joints.
Regular shoulder mobility exercises, even when feeling no symptoms, can help maintain range of motion. Early intervention at the first sign of shoulder stiffness or pain is crucial.
Working closely with healthcare providers to manage both diabetes and shoulder health is the best preventive approach.

