What Is Osteoarthritis?
Osteoarthritis is the most common form of arthritis, affecting approximately 10% of the global population.
This degenerative joint disease impacts both men and women, though women tend to have higher rates of osteoarthritis. The condition becomes significantly more prevalent after age 50.
Osteoarthritis affects the entire joint structure, including surrounding muscles, tendons, joint capsule, and the cartilage inside. As the disease progresses, the protective cartilage covering the bones inside joints gradually wears away, eventually leading to bone-on-bone contact.
This creates painful sensations when weight is placed on affected joints during activities like walking, standing, and climbing stairs.
While osteoarthritis can impact virtually any joint in the body, it most commonly develops in the knees, hips, spine, and hands.
Read more: Which Orthopedic Doctor in Singapore Should You Consider?
Understanding Knee Osteoarthritis
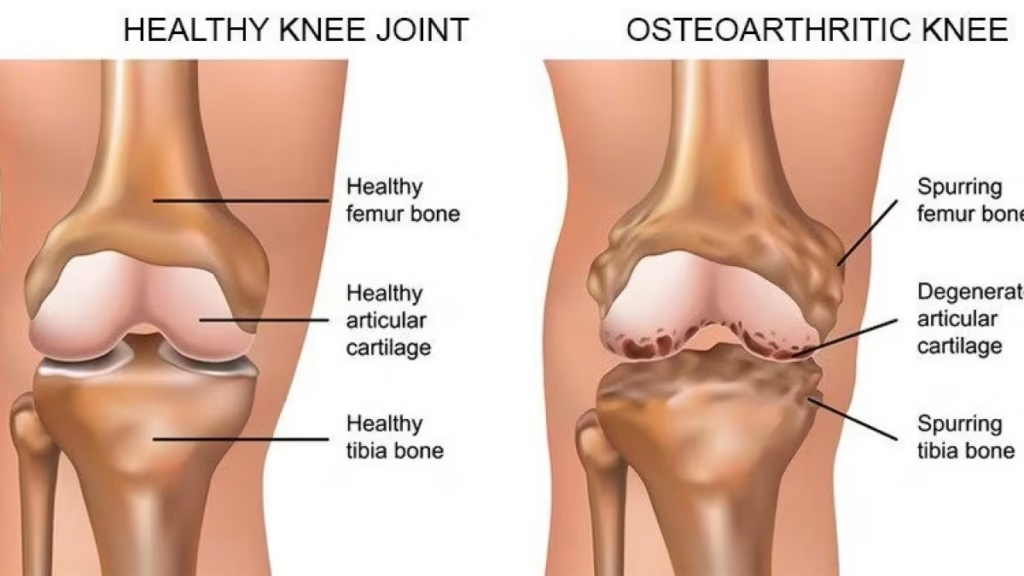
Knee osteoarthritis is the most prevalent type of osteoarthritis and a leading cause of disability. It occurs when the articular cartilage (the smooth lubricating layer covering the ends of bones forming the knee joint) deteriorates.
In severe cases, bones may rub directly against each other with minimal lubrication, causing significant pain and disability.
The condition results when lubricating joint fluid that protects and cushions bones gradually diminishes, losing its shock-absorbing properties.
This leads to increased friction and surrounding bone edema, causing joint pain, stiffness, and reduced mobility.
Read more: Best Orthopedic Doctor in JB for Singaporeans
Symptoms of Osteoarthritis
The primary symptom of osteoarthritis is pain around affected joints after periods of prolonged or strenuous use, such as after extended walking, exercise, or repetitive activities.
Initially, this pain often comes and goes in a predictable pattern, typically increasing with continued joint use but subsiding after sufficient rest periods.
However, as the condition progresses over time, the pain may become more persistent and occur even during lighter activities or at rest.
Other common symptoms include mild stiffness when joints have been rested, known as “gelling,” which makes it difficult to move smoothly after sitting still for extended periods or upon waking.
Many patients experience morning stiffness that can last from several minutes to an hour, often accompanied by swelling around the affected joints.
A warm sensation in the joint area is frequently reported, along with visible joint swelling that may fluctuate throughout the day.
Weather changes, particularly drops in barometric pressure or increased humidity, often worsen pain and stiffness in many patients.
Over time, the structural changes in the joint can lead to the development of crooked-looking joints, which is particularly noticeable in knee joints that may gradually become bow-legged as cartilage wears away unevenly.
Crepitus, characterized by cracking, grinding, or popping noises during joint movements, becomes increasingly common as cartilage deteriorates and bone surfaces begin to rub together.
The appearance of bumps or nodes around affected joints, especially in the fingers, may develop as the condition advances.
Additionally, many patients experience joint instability, where the joint feels loose or unreliable during movement, and occasional locking sensations where the joint temporarily becomes stuck in one position before releasing.
Related article: Total Knee Replacement Surgery in Singapore
Risk Factors and Causes
Several factors contribute to the development of osteoarthritis:
- Age: Risk increases significantly after 50 years
- Sex: Women have higher rates than men
- Body weight: Overweight and obesity are primary risk factors, as each additional kilogram multiplies the pressure on weight-bearing joints
- Previous joint injuries: Past trauma, fractures, or injuries involving joints
- Muscle weakness: Particularly around affected joints
- Occupational factors: Heavy manual labor and repetitive joint stress
- Bone deformities: Abnormally shaped joints like hips and knees place added stress on these structures
- Genetic and family history: Hereditary factors may predispose some individuals
- Other forms of arthritis: Conditions like rheumatoid arthritis or psoriatic arthritis can cause secondary joint damage
You might like: Knee Pain in Singapore: Causes, Treatment & Prevention
Diagnosis of Osteoarthritis
If you experience symptoms consistent with osteoarthritis, healthcare providers can typically confirm the diagnosis through a detailed patient history and symptom evaluation, physical examination of affected joints, and X-rays, which may show characteristic joint changes.
Occasionally, additional tests may be required to exclude other conditions, including joint aspiration to obtain fluid samples from affected joints, magnetic resonance imaging (MRI) to better visualize joint structures, and blood and joint fluid tests to rule out other types of arthritis or systemic diseases.
Treatment Options for Osteoarthritis in Singapore
Currently, there is no cure for osteoarthritis, making ongoing research essential. Treatment focuses on alleviating symptoms, regaining lost muscle strength, and in some cases, surgical intervention.
Non-Surgical Treatments
Physical Therapy and Exercise
Exercise is crucial for building strength in muscles surrounding affected joints, which helps to better support the joint and reduce stress.
Contrary to common misconceptions, appropriate exercise does not worsen osteoarthritis—in fact, a sedentary lifestyle weakens supporting muscles, making joints more vulnerable.
Physiotherapists can assess muscle and joint conditions, design appropriate exercise regimens, reduce pain and swelling, improve range of motion through stretching and strengthening exercises, and help regain functional movement.
Recommended exercises include swimming (generally considered the gentlest option for arthritis), cycling, brisk walking, and slow jogging if appropriate.
Specific stretching exercises for affected areas are also beneficial, particularly for knee osteoarthritis, including quadriceps stretching, hamstring stretching, and calf stretching, along with strengthening exercises targeting quadriceps, hip muscles, and buttock muscles.
Keys to success with exercise therapy are proper guidance, discipline, and perseverance.
You might be interested: Arthritis Treatment in Singapore: Causes, Risks, Symptoms
Medication
Various medications can help manage osteoarthritis symptoms. Topical treatments such as creams, balms, ointments, and adhesive patches provide safe, localized pain relief.
Paracetamol (Panadol) is often prescribed for mild pain, while non-steroidal anti-inflammatory drugs (NSAIDs) are used for more severe pain as they target the inflammatory pathway. COX-2 inhibitors may be prescribed for moderate to severe pain.
Supplements like glucosamine and chondroitin may provide symptomatic relief for some patients, though they do not prevent cartilage deterioration. Always consult with a healthcare provider before starting any medication regimen.
Related article: Scoliosis Treatment in Singapore: Causes and Symptoms
Joint Injections
Several types of injections may provide temporary relief:
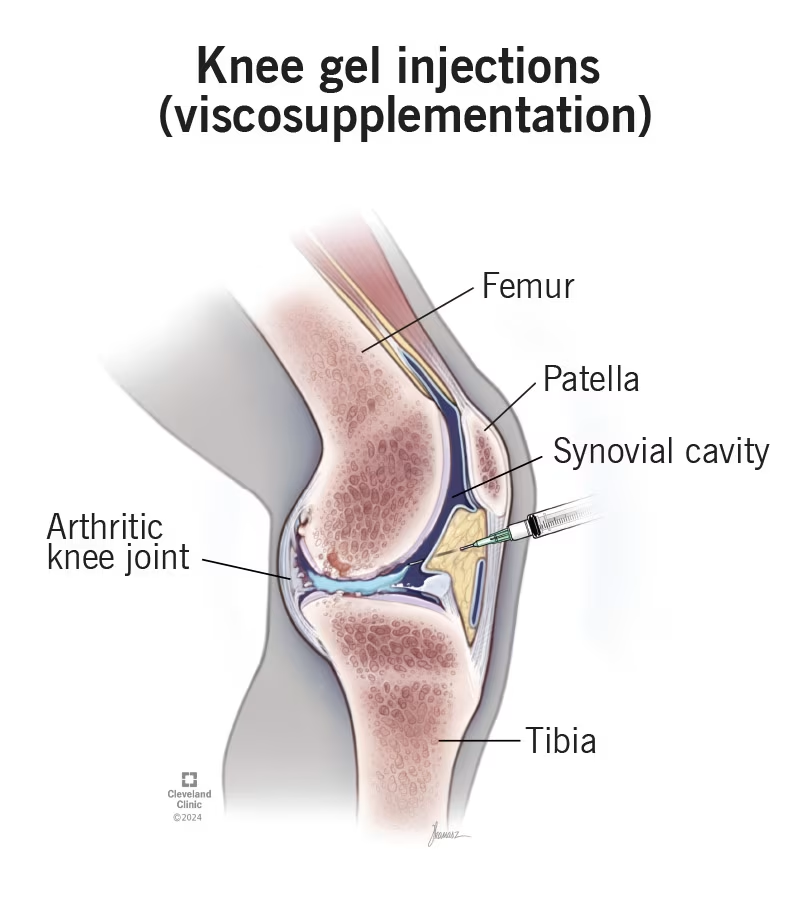
- Lubricant/Viscosupplement Injections:
- Hyaluronic acid derivatives are injected into the joint
- May provide cushioning and lubrication
- Effects typically last up to five months
- More beneficial for younger patients needing temporary relief for increased exercise
- Steroid Injections:
- Can reduce inflammation and pain
- Effects are usually shorter-lasting than lubricant injections
- Repeated steroid injections are generally not recommended
- Platelet-Rich Plasma (PRP):
- Commonly used for pain caused by torn meniscus and osteoarthritis
- Injection sites include the meniscus and surrounding ligaments
- Specialized Gel Injections:
- Some clinics in Singapore offer proprietary gel injections that identify different pain generators in addition to addressing joint inflammation
- These combined approaches aim to provide longer-lasting pain relief
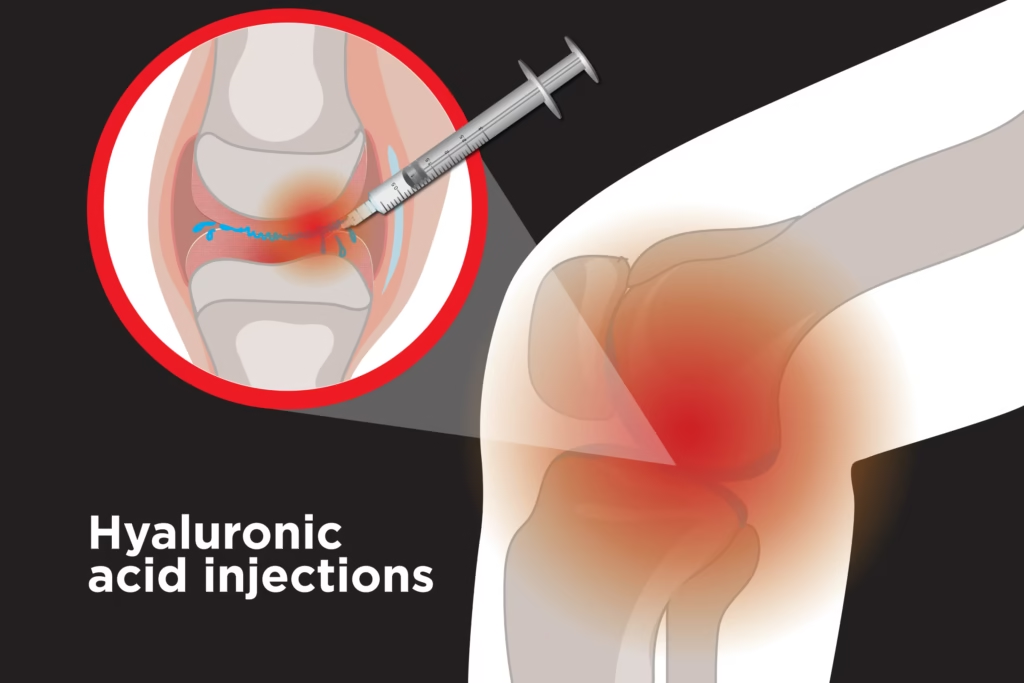
Each injection into joints carries a small risk of infection, so these interventions should be used judiciously.
You might like: Hip Replacement Surgery in Singapore: Cost, Risks
Supportive Devices
Knee braces may be used temporarily to limit joint movement, provide structural support, reduce pain, and minimize stimulation of inflamed muscles.
Self-Care Treatments
Important self-care strategies include weight management to reduce pressure on weight-bearing joints, strengthening lower limbs to better handle daily activities, applying ice packs to reduce swelling after prolonged standing or walking, monitoring and controlling blood sugar levels, and addressing pain promptly before it becomes severe.
Surgical Treatment Options
For patients who do not respond adequately to conservative treatments, several surgical options may be considered.
Arthroscopic Debridement
This minimally invasive “keyhole” procedure involves using an arthroscope to visualize the joint interior, shaving away damaged cartilage, stimulating healing by creating small holes in the bone, and cleaning up damaged portions of the joint.
This approach is typically more suitable for early-stage osteoarthritis.
Osteotomy
This procedure is generally recommended for younger patients (under 50) with limited osteoarthritis.
During an osteotomy, bones around the joint are cut, joint alignment is corrected to redistribute weight-bearing forces, and symptom relief may last up to 10 years.
Joint Replacement Surgery
For advanced osteoarthritis with severe joint damage, joint replacement may be the most effective option.
Total Knee Replacement (TKR) replaces both the medial and lateral compartments of the knee, and sometimes the patellofemoral compartment, with metal and plastic components replacing damaged joint surfaces. This is most appropriate for patients with extensive joint damage.
Unicompartmental (Partial) Knee Replacement replaces only the most damaged compartment, typically the medial compartment, and is less invasive than total knee replacement, suitable for patients with damage limited to one part of the joint.
Joint Fusion (Arthrodesis) is used for some joints, particularly in the hands, where arthritic surfaces are removed and bones on either side are fused, eliminating movement but providing pain relief and stability.
Important considerations for joint replacement include that metal implants also undergo wear and tear, typically lasting 8-12 years depending on lifestyle, posture, and use.
The common practice is to delay knee replacement as long as possible to avoid revision surgeries, with the goal often being to ensure only one knee replacement is needed during a patient’s lifetime.
Prevention Strategies
While osteoarthritis cannot be completely prevented, several measures can help reduce risk and slow progression.
These include maintaining a healthy body weight to minimize stress on weight-bearing joints, engaging in regular moderate exercise to strengthen supporting muscles, following a nutritious balanced diet, preventing joint injuries whenever possible, staying active with appropriate activities, controlling blood sugar levels, and addressing joint pain promptly rather than ignoring symptoms.
When to Seek Medical Attention
You should consult with a healthcare provider when experiencing pain on the front, back, or sides of the knee or other joints, joint deformation, difficulty walking or feeling joint instability, problems with everyday activities like wearing clothes or getting in and out of vehicles, unbalanced or restricted joint movements, persistent swelling in affected areas, or pain that occurs with activity but not at rest.
FAQ
What is the difference between osteoarthritis and other types of arthritis?
Osteoarthritis is primarily a degenerative joint disease caused by wear and tear, aging, and mechanical factors.
Other forms of arthritis, such as rheumatoid arthritis or psoriatic arthritis, are inflammatory conditions with different underlying causes, typically involving the immune system attacking joint tissues.
While all forms can cause joint pain and damage, their treatments and progression differ significantly.
Osteoarthritis is much more common, affecting about 10% of the population, while inflammatory arthritis types are relatively uncommon.
Can osteoarthritis be cured?
Currently, there is no cure for osteoarthritis. Treatment focuses on symptom management, slowing disease progression, and improving joint function through a combination of non-surgical approaches and, when necessary, surgical interventions.
Research continues to explore potential curative treatments, but prevention and early management remain the best strategies for limiting the impact of this condition.
How effective are supplements like glucosamine and chondroitin for treating osteoarthritis?
The evidence for glucosamine and chondroitin supplements is mixed. Some patients report symptomatic relief from these supplements, but they do not prevent cartilage deterioration or modify the disease course.
Their effectiveness tends to be temporary, and they are less likely to help patients with severe osteoarthritis.
It’s advisable to consult with a healthcare provider before starting these supplements, as they may interact with other medications.
What makes knee osteoarthritis more common than other joint types?
Knee osteoarthritis is particularly common because the knee joints bear significant weight and experience substantial mechanical stress during daily activities.
With each step, the load on knee joints can be up to four times a person’s body weight. Additionally, the knee is a complex joint with multiple compartments and surfaces that can wear unevenly.
Previous injuries, alignment issues, and the knee’s crucial role in mobility make it especially vulnerable to osteoarthritic changes compared to other joints.
What are the latest treatment innovations for osteoarthritis in Singapore?
Some of the newer approaches available in Singapore include proprietary gel injections that target multiple pain generators beyond just joint inflammation, platelet-rich plasma therapy, and advanced minimally invasive surgical techniques.
Comprehensive rehabilitation programs that combine various therapeutic approaches are also becoming more prevalent.
For the most current treatment options, it’s best to consult with healthcare providers who specialize in osteoarthritis management.
How long do knee replacements typically last?
Knee replacement implants generally last between 8-12 years, though this can vary significantly based on factors such as the patient’s age, activity level, weight, and surgical technique.
Modern implant materials and designs have improved longevity in many cases.
The common medical practice is to delay knee replacement as long as reasonably possible, especially for younger patients, to minimize the need for revision surgeries later in life.
Is walking good for knee osteoarthritis?
Yes, walking at a moderate pace is generally beneficial for knee osteoarthritis when done appropriately.
Walking strengthens the muscles around the knee, improves joint lubrication, and helps maintain mobility.
However, the intensity should be adjusted based on pain levels, and proper footwear with good cushioning is important.
If walking causes significant pain that persists for hours afterward, it’s advisable to consult with a healthcare provider or physiotherapist to modify the walking program or consider alternative exercises.
Can weight loss really help with osteoarthritis symptoms?
Weight loss can significantly improve osteoarthritis symptoms, particularly in weight-bearing joints like the knees and hips.
Even modest weight reduction can substantially decrease the pressure on these joints.
Research shows that for every kilogram of weight loss, there is a four-fold reduction in the load exerted on the knee for each step taken.
Many patients report noticeable pain reduction and improved mobility after losing weight, making this one of the most effective non-surgical interventions for osteoarthritis management.
What should I expect during physical therapy for osteoarthritis?
During physical therapy for osteoarthritis, you can expect a comprehensive approach that begins with an assessment of your joint condition, pain levels, and functional limitations.
Treatment typically includes a combination of pain management techniques, specific exercises to improve strength and flexibility, education about joint protection, and potentially hands-on therapeutic techniques.
Your physiotherapist will create a personalized exercise program that you’ll perform both during sessions and at home. Consistency with home exercises is crucial for achieving optimal results from physical therapy.
How can I tell if my joint pain is osteoarthritis or something else?
Osteoarthritis typically develops gradually and is characterized by pain that worsens with activity and improves with rest, at least in the early stages.
Morning stiffness usually lasts less than 30 minutes, and there may be crepitus (cracking or grinding sensations) with joint movement.
By contrast, inflammatory arthritis often causes prolonged morning stiffness, may affect multiple joints symmetrically, and can include systemic symptoms like fatigue.
Other conditions such as gout cause sudden, intense pain often with redness and warmth. For an accurate diagnosis, it’s important to consult a healthcare provider who can perform appropriate examinations and tests.

