Knee pain is an increasingly common health concern in Singapore, particularly affecting individuals over the age of 40.
Studies show that among Singaporeans, the prevalence is highest among Indians, followed by Malays and Chinese.
As the largest joint in the human body, the knee plays a crucial role in mobility and daily activities, making knee pain a significant issue that can substantially impact quality of life.
Often described as “creaky knees,” knee problems represent the most common age-related musculoskeletal condition in Singapore.
Whether you’re experiencing occasional twinges or chronic discomfort, understanding the causes, symptoms, and treatment options is essential for managing knee health effectively.
Read more: Total Knee Replacement Surgery in Singapore
Understanding Knee Anatomy
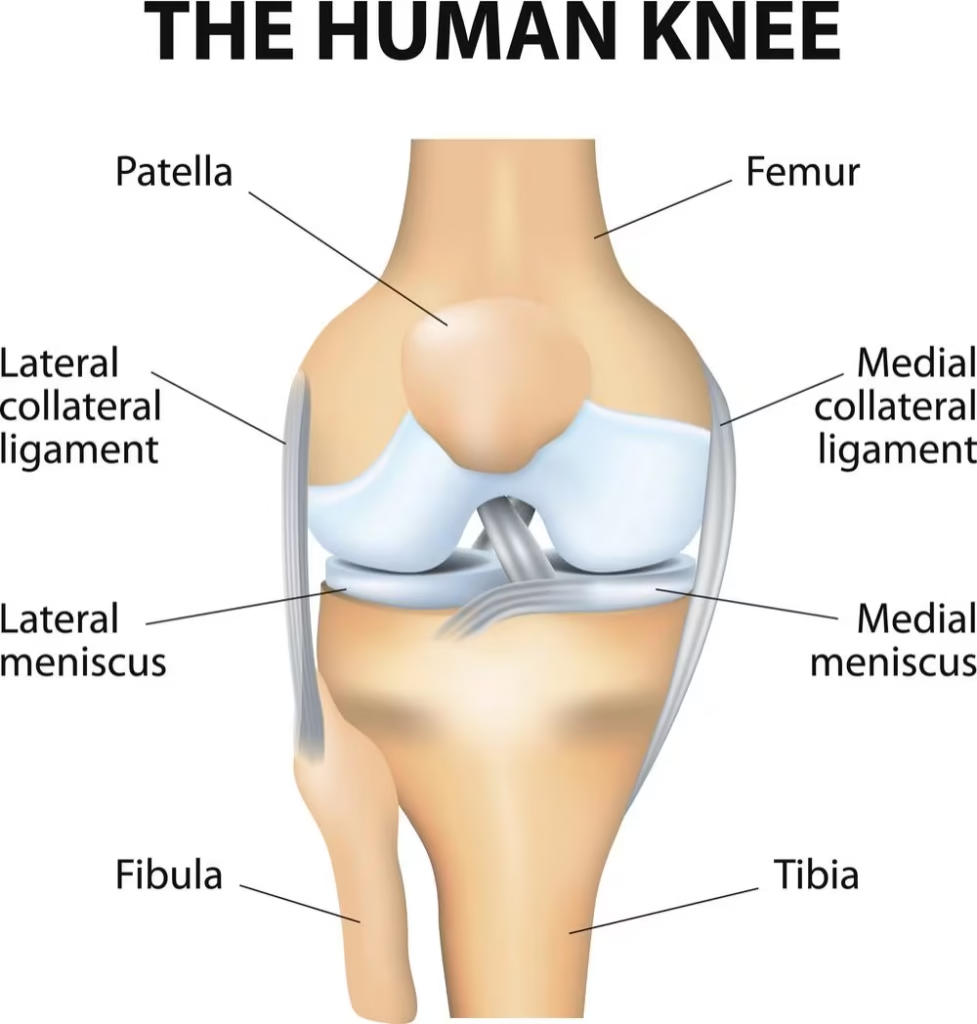
To comprehend knee pain, it’s important to first understand the knee’s complex structure. The knee joint connects three bones:
Supporting this joint is an intricate network of:
- Ligaments: Provide stability (including the crucial anterior cruciate ligament or ACL)
- Tendons and muscles: Enable movement
- Menisci: Two C-shaped cartilage discs that serve as shock absorbers
- Bursae: Fluid-filled sacs that help the knee move smoothly
Like any mechanical system, the knee experiences wear and tear over time. This natural deterioration accelerates with factors like excess weight, high-impact activities, and aging.
As we grow older, our knees also become more susceptible to inflammatory and crystal-related diseases.
Read more: Arthritis Treatment in Singapore: Causes, Risks, Symptoms
Common Symptoms of Knee Pain
Knee pain manifests through various symptoms that can signal different underlying conditions and may significantly impact daily activities and quality of life.
The most common presentations include joint pain or aches around the knee area, which can range from mild discomfort to severe, debilitating pain that interferes with normal function.
Many patients experience morning stiffness that typically lasts for brief periods after waking, reflecting the joint’s need to “warm up” after periods of inactivity.
Mild swelling around the knee joint is frequently observed and may fluctuate throughout the day depending on activity levels and positioning.
Painful clicking or popping sounds during movement, known as crepitus, often indicate changes in joint surfaces or cartilage damage.
Patients commonly report pain during specific activities such as squatting or climbing stairs, with symptoms typically improving during periods of rest.
Reduced range of motion in the knee joint and difficulty bending the knee can significantly impact mobility and independence.
Many individuals describe sensations of the knee “giving way” or feeling unstable, which can create anxiety about walking or participating in physical activities.
Visible changes such as redness or warmth around the knee joint may indicate inflammation or infection requiring medical attention.
Aching or pain when weight is placed on the affected knee can make walking, standing, or climbing stairs particularly challenging.
These symptoms typically develop gradually over time and may worsen with prolonged walking or standing activities.
For some individuals, symptoms might appear suddenly following an acute injury, while for others, they develop slowly over months or years as part of age-related degeneration or cumulative wear and tear.
Read more: Osteoarthritis Treatment in Singapore: Symptoms, Prevention
Common Risk Factors
SSeveral factors can significantly increase your risk of developing knee pain, and understanding these risk factors can help individuals take preventive measures and seek appropriate care when needed.
Age represents a major risk factor, particularly for people over 40 years old, as the natural aging process leads to gradual deterioration of cartilage and other joint structures.
Being overweight places additional mechanical stress on knee joints during daily activities, accelerating wear and tear while increasing the risk of developing osteoarthritis.
Psychological factors including poor sleep quality, low mood, and anxiety can amplify pain perception and create a cycle where pain affects mental health, which in turn increases the subjective experience of pain.
Activity levels play a crucial role, as both overloading joints with excessive high-impact activities and insufficient activity that leads to muscle weakness can negatively impact knee health.
Previous knee injuries such as ligament tears, meniscus damage, or fractures create areas of weakness and increase the likelihood of developing chronic pain or arthritis later in life.
Muscle weakness, particularly in the hip and knee stabilizing muscles, reduces the joint’s natural protection and support system.
Genetic factors and family history of knee problems can predispose individuals to developing similar conditions, though lifestyle modifications can still significantly influence outcomes.
Participation in high-impact sports including basketball, soccer, or running places repetitive stress on knee structures and increases injury risk, particularly when proper conditioning and technique are lacking.
Occupational factors such as jobs requiring frequent kneeling, squatting, or heavy lifting create cumulative stress on knee joints over time, making workplace ergonomics and protective measures important considerations for long-term joint health.
You might like: Sports Doctors in Singapore: Guide to Finding a Suitable Specialist
When to Consult a Doctor
While mild knee pain often resolves with rest and self-care, certain symptoms warrant prompt medical attention:
- Hot and swollen knee, with or without fever
- Severe fall, trauma, or impact that limits knee movement
- Joint stiffness in the morning lasting more than 30 minutes
- Rapid worsening of knee pain
- Inability to bear weight on the affected leg
- Visible deformity or significant swelling
- Popping sound at the time of injury accompanied by immediate swelling
- Pain that doesn’t improve after several days of rest and over-the-counter pain medication
Early consultation can prevent further damage and improve treatment outcomes. If you experience any of these warning signs, seek medical advice promptly.
This might help: Which Orthopedic Doctor in Singapore Should You Consider?
Common Types of Knee Conditions
Osteoarthritis
The most prevalent form of arthritis, osteoarthritis develops due to progressive wearing down of cartilage over time.
This degenerative disease limits range of motion and triggers pain, stiffness, weakness, and swelling of the knee.
Risk factors include advanced age, excess weight, and genetic predisposition.
According to the World Health Organization, approximately 40% of people over 70 will develop osteoarthritis.
Rheumatoid Arthritis
Unlike osteoarthritis, rheumatoid arthritis is an autoimmune disease where the body’s immune system attacks the knee joint lining.
This causes the tissue around the joint to become inflamed and thickened, potentially damaging and reducing knee cartilage over time.
This might help: Best Orthopedic Doctor in JB for Singaporeans
Anterior Cruciate Ligament (ACL) Injury
The ACL is one of the main stabilizing ligaments in the knee. ACL tears commonly occur during sports involving sudden stops, pivots, or direction changes.
Activities like football, netball, tennis, dancing, and skiing pose higher risks for ACL injuries.
Symptoms of an ACL tear include:
- Immediate pain
- Audible popping sound
- Difficulty moving the knee
- Joint instability
- Rapid swelling (immediate or within hours)
Related article: ACL Reconstruction Surgery in Singapore: Causes, Costs
Meniscus Tear
The meniscus is a C-shaped cartilage that cushions the knee joint. Tears typically occur during forceful rotation movements while the foot remains planted—common in basketball or football. Aging can also make the meniscus more vulnerable to tears.
Signs of a meniscus tear include:
- Clicking or popping sounds during movement
- Locking sensation (inability to straighten the knee)
- Swelling or tenderness along the joint line
- Pain on either side of the knee
- Limited range of movement
Patellar Tendonitis
Also known as “jumper’s knee,” patellar tendonitis involves inflammation of the tendon connecting the kneecap to the shinbone. This condition is common among athletes engaged in jumping or repetitive running.
Characteristic symptoms include:
- Pain and tenderness just below the kneecap
- Pain and swelling when kneeling
- Worsening pain during physical activity
Bursitis
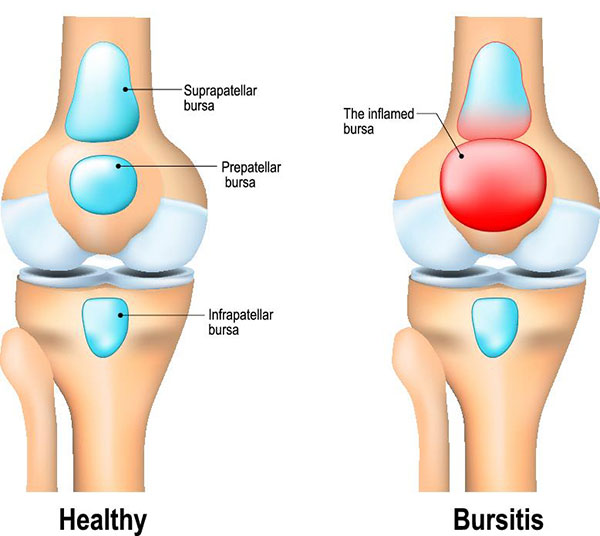
When the fluid-filled sacs (bursae) that cushion the knee become irritated, usually due to repetitive bending or kneeling, bursitis develops. This condition—sometimes called “housemaid’s knee”—causes pain and swelling, particularly during movement.
Gout
Crystal deposits within the joint cause pain, swelling, and inflammation (with visible redness and warmth).
Age, genetics, and obesity predispose individuals to gout, while excessive alcohol consumption and kidney disease represent additional risk factors.
Patellofemoral Pain Syndrome
Also known as “runner’s knee,” this condition results from poor alignment of the kneecap relative to the thigh bone.
It may develop due to weak thigh muscles or activities that stress the knee, especially twisting movements.
Being overweight or engaging in frequent running or squatting can exacerbate the condition.
Diagnosis Methods
Proper diagnosis begins with a thorough physical examination to identify the cause of knee pain. Your healthcare provider will:
- Review your medical history and symptom patterns
- Perform physical tests to check bone alignment, muscle strength, and joint stability
- Assess your range of motion and locate areas of tenderness
- Sometimes request imaging tests such as:
- X-rays to show bone damage or alignment issues
- MRI scans to visualize soft tissue injuries affecting cartilage, ligaments, or tendons
- Occasionally, blood tests or joint fluid analysis to rule out infection or inflammatory conditions
An accurate diagnosis is essential for developing an effective treatment plan tailored to your specific condition.
Treatment Options
Treatment for knee pain depends on its cause and severity. Your healthcare provider will recommend a customized approach that may include:
Non-Surgical Approaches

- Rest and activity modification: Temporarily avoiding activities that worsen pain
- Ice and heat therapy: Ice helps reduce swelling and inflammation, while heat can relieve stiffness
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation
- Physical therapy: Exercises to strengthen muscles around the knee, improve flexibility, and enhance joint stability
- Braces or supports: Providing structural support and improved alignment
- Weight management: Reducing stress on the knee joints
- Injections: Corticosteroid injections to reduce inflammation or hyaluronic acid to improve joint lubrication
- Alternative therapies: Some patients find relief with acupuncture or supplements like glucosamine (though evidence for their effectiveness varies)
Surgical Options
When conservative treatments fail to provide relief, surgical interventions may be considered:
- Arthroscopic surgery: A minimally invasive procedure using a small camera and instruments inserted through tiny incisions. This approach can repair damaged ligaments or meniscus, remove loose bodies, and reconstruct cartilage. Recovery is typically faster than with traditional surgery.
- Knee replacement surgery: The surgeon removes damaged portions of the knee and replaces them with artificial components made from metal and plastic. This may involve:
- Partial knee replacement (replacing only the most damaged sections)
- Total knee replacement (replacing the entire joint)
According to research, about 90% of knee replacement patients can resume normal activities, while some may still experience occasional discomfort or require revision surgery. Notably, 85% of artificial knees remain functional after 20 years.
Lifestyle Changes and Prevention Strategies
Whether you’re managing existing knee pain or aiming to prevent future issues, these lifestyle modifications can help:
1. Maintain a Healthy Weight
Excess weight places significant additional stress on knee joints. Each extra kilogram increases the force on your knees during everyday activities like walking and climbing stairs.
2. Exercise Appropriately
- Strengthen supporting muscles: Focus on exercises that build strength in the quadriceps, hamstrings, and other knee-supporting muscles
- Low-impact activities: If you’re just beginning an exercise program, start with gentler options like walking, swimming, or cycling
- Gradual progression: Increase workout intensity slowly to avoid strain
- Complete regular stretching: Maintain flexibility around the joint
- Mixed activity types: Include a combination of strength, balance, and flexibility exercises at least 3 days weekly
- Stop if pain occurs: Don’t push through knee pain during exercise
3. Use Proper Footwear
Choose shoes with adequate cushioning and arch support to distribute pressure evenly and minimize knee impact. Replace worn-out shoes regularly to maintain proper shock absorption.
4. Check Your Gait
Your walking style may put your knee out of alignment, adding uneven stress. A physical therapist can evaluate your gait and suggest corrections if needed.
5. Consider Supportive Equipment
- Knee braces or sleeves: These compress and align the knee while offering support
- Arch supports: May help relieve knee pain by improving foot alignment
- Knee pads: If your activities involve frequent kneeling, padding helps prevent bursitis
6. Address Pain Early
Don’t ignore minor knee discomfort. Early intervention often prevents the development of more serious conditions and chronic pain patterns.
Managing Knee Pain at Home
For mild to moderate knee pain, several home remedies may provide relief:
- Compression bandages: Elastic knee bands can help with swelling and knee alignment while offering support
- Rest: Sometimes simply elevating your legs relieves pressure and reduces pain
- Ice therapy: Applying ice can numb pain and reduce swelling and inflammation
- Gentle stretching: Maintains flexibility and range of motion
- Over-the-counter pain relief: Used according to instructions and for limited periods
Comprehensive FAQ Section
What causes knee pain to worsen at night?
Knee pain often intensifies at night due to several factors. When you’re less active, inflammation can settle in the joint, and without the distraction of daily activities, pain perception increases.
Additionally, lying in certain positions may put pressure on already sensitive areas.
Try placing a pillow between your knees when sleeping on your side, applying ice before bedtime, and ensuring your mattress provides adequate support to minimize nighttime discomfort.
How effective are knee braces for pain relief?
Knee braces can be quite effective for certain conditions by providing stability, improving alignment, and reducing strain on damaged structures.
They work by limiting harmful movements while allowing beneficial ones.
For osteoarthritis, unloader braces that shift weight away from damaged areas can reduce pain by 30-50% in many patients.
However, braces work best as part of a comprehensive treatment plan that includes physical therapy and appropriate activity modification rather than as a standalone solution.
Can glucosamine supplements actually help with knee pain?
The evidence for glucosamine is mixed. Some studies suggest that glucosamine and chondroitin supplements may provide modest pain relief for some individuals with osteoarthritis, potentially by reducing inflammation and supporting cartilage repair mechanisms.
However, clinical trials show inconsistent results, with some people experiencing significant improvement while others notice little difference.
These supplements appear most effective when taken consistently for at least 2-3 months.
If you’re considering glucosamine, discuss it with your healthcare provider, especially if you have shellfish allergies, as many glucosamine products derive from shellfish.
What exercises should I avoid if I have knee pain?
With knee pain, it’s generally wise to avoid high-impact activities that place excessive stress on the joint.
These include deep full squats, lunges with improper form, high-impact jumping exercises, running on hard or uneven surfaces, and activities involving sudden pivoting movements.
Also, avoid exercises that cause pain during or after the activity. Instead, focus on low-impact alternatives like swimming, cycling on a properly fitted bike, controlled partial squats, and straight leg raises that strengthen supporting muscles without aggravating the joint.
How does excess weight specifically affect knee health?
Excess weight dramatically increases the load on your knee joints.
Research shows that for every pound of body weight, your knees experience approximately 4-6 pounds of pressure during walking and up to 10 pounds when climbing stairs or running.
This means even modest weight gain significantly increases joint stress.
Additionally, fat tissue produces inflammatory chemicals that can further damage joint tissues over time.
Studies indicate that losing just 10% of body weight can reduce knee pain by 50% in overweight individuals with osteoarthritis, making weight management one of the most effective interventions for knee health.
When is knee replacement surgery necessary?
Knee replacement surgery becomes a consideration when severe pain and limited function persist despite conservative treatments like physical therapy, medications, injections, and activity modifications.
Appropriate candidates typically experience pain that interferes with daily activities, pain at rest or at night, and significant joint deformity or instability.
Most patients have advanced osteoarthritis visible on X-rays showing substantial joint space narrowing.
The decision timing varies by individual, but generally, surgery is recommended when quality of life is significantly impaired and non-surgical options have been exhausted.
The average age for knee replacement is between 65-70, though younger patients may qualify based on symptom severity.
How does menopause affect knee pain in women?
Menopause can significantly impact knee health due to hormonal changes.
Declining estrogen levels affect joint tissues, as estrogen helps maintain cartilage and reduce inflammation.
Without adequate estrogen, women often experience increased joint inflammation and accelerated cartilage degeneration.
Additionally, hormonal changes during menopause frequently lead to weight gain and altered fat distribution, placing additional stress on the knees.
Bone density reductions associated with menopause can also affect the knee joint structure.
Women experiencing menopausal joint discomfort may benefit from weight-bearing exercises to maintain bone density, anti-inflammatory foods, and discussing hormone replacement therapy options with their healthcare provider.
What’s the difference between runner’s knee and jumper’s knee?
Though both affect active individuals, runner’s knee (patellofemoral pain syndrome) and jumper’s knee (patellar tendonitis) are distinct conditions.
Runner’s knee involves pain around or behind the kneecap when the patella tracks improperly against the femur, often during repetitive motion like running.
It typically causes diffuse pain and grinding sensations. In contrast, jumper’s knee is inflammation of the patellar tendon connecting the kneecap to the shinbone, resulting from repetitive jumping activities.
It causes specific, localized pain just below the kneecap that worsens with activities that load the tendon, like jumping or climbing stairs.
Treatment approaches differ, highlighting the importance of accurate diagnosis for effective management.
How long does it typically take to recover from arthroscopic knee surgery?
Recovery from arthroscopic knee surgery varies based on the specific procedure performed.
For minor procedures like débridement (removal of damaged tissue), patients often resume normal walking within 1-2 weeks and return to most activities within 6-8 weeks.
Meniscus repairs typically require 4-6 weeks before returning to light activities, with full recovery taking 3-4 months.
ACL reconstructions demand more extensive rehabilitation, with patients returning to normal walking in about 2-4 weeks but requiring 6-9 months before returning to sports.
Throughout recovery, physical therapy plays a crucial role in restoring strength and function. Following your surgeon’s post-operative guidelines closely optimizes healing and minimizes complications.
Can knee pain be related to problems in other joints?
Yes, knee pain can definitely stem from issues in other joints, particularly the hip and ankle. This relationship, known as the kinetic chain effect, occurs because these joints work together during movement.
Hip problems often cause compensatory movements that place abnormal stress on the knee. For example, weakness in hip abductor muscles can lead to improper knee alignment during walking.
Similarly, ankle instability or limited mobility may alter gait patterns, transferring excessive forces to the knee joint. Even lower back problems can refer pain to the knee area.
Comprehensive treatment should consider this interconnectedness, sometimes addressing problems in multiple joints to fully resolve knee pain.
Conclusion
Knee pain represents a significant health concern in Singapore, particularly as the population ages.
With proper understanding of risk factors, symptoms, and treatment options, many individuals can effectively manage their condition and maintain an active lifestyle.
Early intervention is key—don’t wait until pain becomes severe before seeking help.
By combining medical treatment with appropriate lifestyle modifications, most people with knee pain can experience substantial improvement in both symptoms and function.
Whether you’re dealing with existing knee problems or hoping to prevent future issues, the strategies outlined in this guide provide a comprehensive approach to maintaining knee health.
Remember that each person’s situation is unique, so working closely with healthcare providers to develop an individualized plan offers the best path to optimal knee function and quality of life.

