Recovering from angioplasty represents a pivotal moment in your cardiovascular health journey.
While this minimally invasive procedure successfully opens blocked arteries and restores blood flow to your heart, the choices you make at your dinner table will significantly influence your long-term recovery and future heart health.
Your dietary decisions following angioplasty procedure directly impact healing speed, complication prevention, and the likelihood of developing future arterial blockages.
Understanding which foods promote cardiovascular wellness and which ones to eliminate creates the foundation for optimal recovery and sustained heart health.
Read more: Comprehensive Guide to Coronary Angioplasty in Singapore
Understanding Angioplasty and Its Impact on Your Nutritional Needs
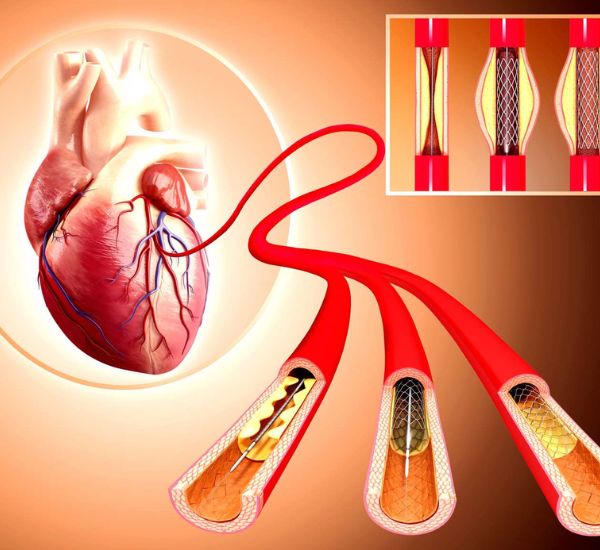
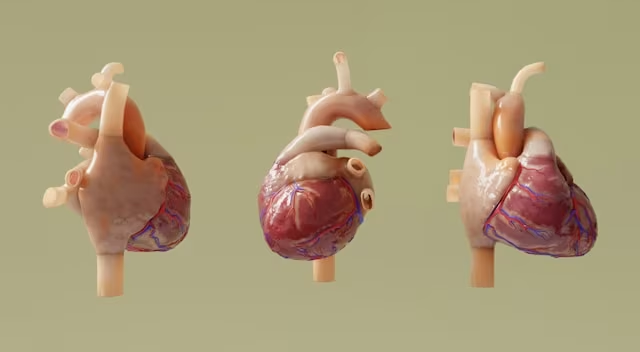
Angioplasty, medically known as percutaneous coronary intervention, involves inserting a balloon-tipped catheter into narrowed coronary arteries.
The balloon inflates to compress plaque buildup against artery walls, often followed by stent placement to maintain vessel openness.
This procedure addresses coronary artery disease, where cholesterol, fat, and other substances accumulate in arterial walls, restricting blood flow to heart muscle.
Following angioplasty, your cardiovascular system requires specific nutrients to support healing while preventing future plaque formation.
The relationship between nutrition and heart health becomes even more critical post-procedure.
Your food choices directly influence inflammation levels, cholesterol production, blood pressure regulation, and overall cardiovascular function. Strategic dietary planning transforms your meals into powerful medicine for your recovering heart.
Read more: Which Cardiologist in Singapore Should You Consider? (Sort by Reviews)
Essential Foods for Post-Angioplasty Recovery
Fruits and Vegetables: Nature’s Heart Medicine
Consuming at least four to five servings of fruits and vegetables daily provides essential vitamins, minerals, and fiber crucial for cardiovascular recovery.
These nutrient-dense foods contain potassium, which counteracts sodium’s effects and helps regulate blood pressure.
When selecting fruits, prioritize fresh options like apples, oranges, bananas, pears, peaches, and berries for maximum nutritional benefit.
If fresh isn’t available, canned varieties without added sugars work well, as do frozen alternatives without syrups. Dried fruits can be included but should be unsweetened versions to avoid excess sugar intake.
For vegetables, fresh selections such as tomatoes, cabbage, carrots, and bell peppers provide optimal nutrition and flavor. Leafy greens including spinach, kale, and romaine lettuce offer exceptional nutrient density.
Cruciferous vegetables like broccoli and cauliflower provide powerful antioxidants. When purchasing canned vegetables, always choose low-sodium varieties to support blood pressure management.
Cranberries deserve special mention for their anti-inflammatory properties and ability to enhance blood vessel dilation.
Berries, in particular, provide powerful antioxidants that combat oxidative stress and support cardiovascular healing.
Related article: Eating Disorder Treatment in Singapore: Causes, Recovery
Whole Grains: Fiber-Rich Foundation
Whole grains serve as excellent sources of B vitamins, fiber, and trace minerals including iron, magnesium, and zinc.
The fiber content specifically helps remove cholesterol from your bloodstream before it can contribute to new plaque formation.
| Whole Grain Type | Key Benefits | Serving Suggestions |
|---|---|---|
| Brown Rice | High fiber, B vitamins | Replace white rice in meals |
| Oats | Beta-glucan fiber, cholesterol reduction | Morning oatmeal, overnight oats |
| Barley | Soluble fiber, heart protection | Soups, grain bowls |
| Quinoa | Complete protein, minerals | Salads, side dishes |
| Whole Wheat | Fiber, nutrients | Bread, pasta alternatives |
Beta-glucan, found abundantly in oats and barley, deserves special recognition for its cholesterol-absorbing properties.
This unique fiber binds to cholesterol in your digestive tract, preventing its absorption into your bloodstream.
Heart-Healthy Proteins and Fats
Cold-water fatty fish provide essential omega-3 fatty acids that reduce inflammation, lower triglycerides, and support healthy heart rhythm.
Research demonstrates consistent omega-3 benefits for reducing both resting and stress-induced heart rates.
Salmon stands out as particularly rich in EPA and DHA omega-3s, while mackerel offers high omega-3 content with versatile preparation options.
Sardines provide a convenient and affordable omega-3 source, herring represents a traditional choice with excellent nutrient profile, and tuna offers a popular option with moderate omega-3 levels.
For those seeking leaner protein options, bass, tilapia, and cod provide lower fat content while remaining nutritious.
Skinless poultry offers lean protein without saturated fat, while legumes such as beans, lentils, and chickpeas provide both protein and fiber.
Tofu and soy products serve as excellent plant-based protein alternatives for those following vegetarian approaches.
Nuts, Seeds, and Heart-Protective Compounds

Extensive research demonstrates that regular nut consumption inversely correlates with cardiovascular disease risk.
Nuts provide multiple heart-protective mechanisms: reducing LDL cholesterol, improving arterial health, decreasing inflammation, and preventing blood clot formation.
Walnuts deserve special recognition for their high alpha-linolenic acid content, a plant-based omega-3 fatty acid. Almonds provide vitamin E, healthy fats, and fiber, while pistachios offer potassium and antioxidants.
Among seeds, sunflower seeds deliver vitamin E and magnesium, flaxseeds provide omega-3s, lignans, and fiber, and chia seeds offer a combination of omega-3s, protein, and minerals.
Consume nuts and seeds in moderate portions (about one ounce daily) due to their caloric density. Choose raw or dry-roasted varieties over salted or flavored options to minimize sodium intake.
Foods to Limit or Avoid During Recovery
Processed and High-Sodium Foods
Processed meats like hot dogs, deli meats, and bacon contain excessive sodium, nitrates, and preservatives that strain your cardiovascular system.
These foods also tend to be high in saturated fats, which can elevate cholesterol levels and promote inflammation.
Foods particularly high in sodium that should be limited include canned soups and broths, packaged snack foods, restaurant meals, frozen dinners, pickled foods, and condiments like soy sauce.
These items can significantly impact blood pressure and fluid retention, complicating your recovery process.
Unhealthy Fats and Refined Carbohydrates
Saturated fats, found in butter, cream, fatty red meat, and full-fat dairy products, can raise LDL cholesterol levels. Trans fats, present in many fried and packaged foods, pose even greater cardiovascular risks.
The American Heart Association recommends limiting saturated fat to 5-6% of daily calories. For a 2000-calorie diet, this equals approximately 120 calories or 13 grams of saturated fat daily.
Refined carbohydrates that should be avoided include white bread and rolls, white rice, regular pasta, sugary cereals, pastries and baked goods, and candy and sweets. These foods lack essential nutrients and can contribute to blood sugar spikes and inflammation.
Added Sugars and Sweetened Beverages
Excessive sugar consumption contributes to weight gain, inflammation, and increased diabetes risk. Limit or eliminate sugary beverages, including sodas, fruit juices, energy drinks, and sweetened coffee beverages.
Evidence-Based Heart-Healthy Diet Approaches
The DASH Diet Approach
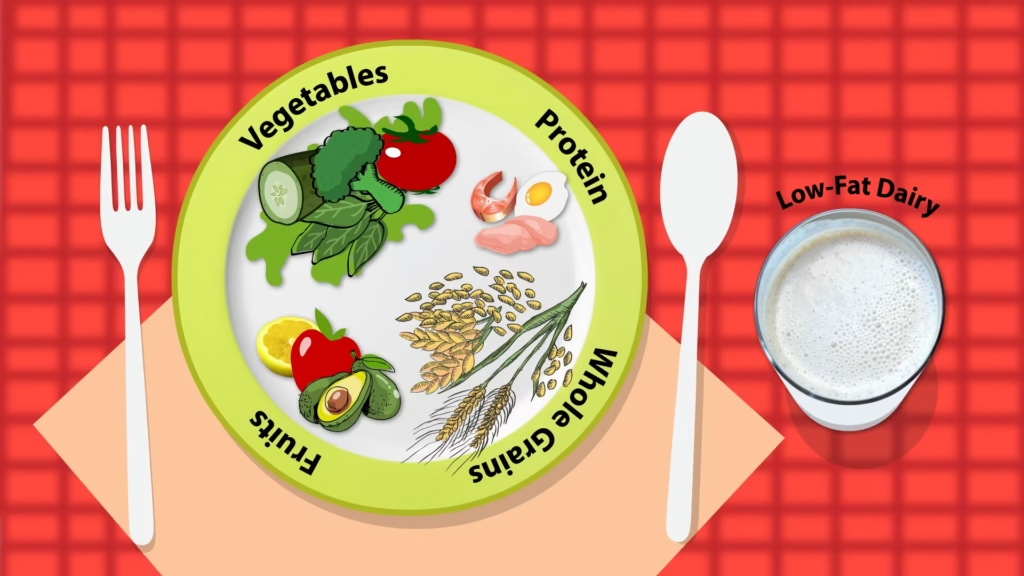
The Dietary Approaches to Stop Hypertension (DASH) diet emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while limiting sodium, sweets, and red meat.
Clinical trials demonstrate DASH diet effectiveness for reducing blood pressure, cholesterol levels, and cardiovascular disease risk.
The DASH approach recommends 4-5 servings each of fruits and vegetables daily, 6-8 servings of whole grains daily, 2-3 servings of low-fat dairy daily, 6 ounces or less of lean meat, poultry, and fish daily, plus 4-5 servings of nuts, seeds, and legumes weekly.
Mediterranean Diet Pattern
The Mediterranean diet emphasizes plant-based foods, olive oil, fish, and moderate wine consumption while limiting red meat and processed foods. This eating pattern provides abundant omega-3 fatty acids, antioxidants, and anti-inflammatory compounds.
Key features of the Mediterranean diet include abundant fruits and vegetables, whole grains and legumes, olive oil as the primary fat source, regular fish and seafood consumption, moderate amounts of poultry and dairy, limited red meat intake, and optional moderate wine consumption.
Recovery Timeline and Dietary Progression
Immediate Post-Procedure (First Week)
During your initial recovery period, focus on easily digestible foods that won’t strain your system. Your healthcare team will provide specific dietary guidelines based on your procedure specifics and overall health status.
Week 1 Recommendations:
- Light, easily digestible meals
- Adequate hydration
- Avoid heavy, greasy foods
- Small, frequent meals
- Monitor for any digestive discomfort
Short-Term Recovery (2-4 Weeks)
Most people begin returning to normal activities during this period. Gradually expand your food choices while maintaining heart-healthy principles.
Weeks 2-4 Focus:
- Introduce more variety in fruits and vegetables
- Incorporate whole grains systematically
- Add omega-3 rich fish twice weekly
- Begin regular physical activity as cleared by your physician
- Establish sustainable eating patterns
Long-Term Maintenance (Beyond 1 Month)
Long-term success requires sustainable lifestyle changes rather than temporary dietary restrictions. Focus on creating enjoyable, heart-healthy meals that you can maintain indefinitely.
Practical Meal Planning Strategies
Effective meal planning begins with establishing consistent weekly preparation habits that support your nutritional goals.
Weekly Meal Preparation Tips
Planning Phase:
To create a sustainable meal planning routine, schedule weekly meal planning sessions at a time that works for your lifestyle. When planning, create grocery lists organized by food categories to make shopping more efficient.
Remember to plan for variety across different food groups to ensure balanced nutrition, and always consider your schedule for cooking time availability throughout the week.
Preparation Techniques:
Successful meal preparation relies on smart time-saving strategies. Batch cook grains and proteins on weekends when you have more time available.
Pre-wash and chop vegetables for easy access during busy weekdays, and prepare healthy snacks in portion-controlled containers to avoid impulsive eating.
Focus on using healthy cooking methods such as baking, grilling, steaming, and sautéing to preserve nutrients and minimize added fats.
Sample Daily Meal Structure
Breakfast Options:
Start your day with nutritious choices like oatmeal topped with fresh berries and chopped walnuts for fiber and healthy fats.
Alternatively, enjoy whole grain toast with creamy avocado and sliced tomato, or try Greek yogurt with fresh fruit and ground flaxseed for protein and omega-3s. For a heartier option, prepare a vegetable omelet served with whole grain toast.
Lunch Ideas:
Midday meals can include a refreshing salmon salad with mixed greens and olive oil dressing, or warm up with lentil soup paired with whole grain crackers.
Create a satisfying quinoa bowl with roasted vegetables, or wrap up turkey and avocado in a whole wheat tortilla for a portable option.
Dinner Suggestions:
End your day with balanced meals such as baked fish served with roasted vegetables and brown rice, or lean chicken accompanied by sweet potato and steamed broccoli.
For plant-based options, try a bean and vegetable stir-fry over quinoa, or enjoy grilled tofu with Mediterranean vegetables for a flavorful and healthy dinner.
Special Considerations and Modifications
Managing Medications and Food Interactions
Certain heart medications may interact with specific foods. Blood-thinning medications, commonly prescribed post-angioplasty, can be affected by vitamin K-rich foods and certain supplements.
Important Medication Considerations:
- Maintain consistent vitamin K intake if taking warfarin
- Avoid grapefruit with certain heart medications
- Limit alcohol consumption, especially with blood pressure medications
- Consult your pharmacist about supplement interactions
Addressing Common Recovery Challenges
Appetite Changes: Some people experience appetite changes following angioplasty. Focus on nutrient-dense foods and smaller, more frequent meals if large portions feel overwhelming.
Digestive Sensitivities: Medications and stress can affect digestion. Choose gentler foods if experiencing stomach upset, and gradually reintroduce higher-fiber foods to prevent digestive discomfort.
Energy Fluctuations: Balanced meals with complex carbohydrates, lean proteins, and healthy fats help maintain steady energy levels throughout your recovery period.
Lifestyle Integration for Long-Term Success
Creating Sustainable Habits
Successful dietary changes require gradual implementation rather than dramatic overhauls. Focus on making one or two changes weekly until they become automatic habits.
Habit Formation Strategies:
- Start with small, achievable changes
- Link new habits to existing routines
- Track progress without obsessing over perfection
- Celebrate small victories along the way
Social and Cultural Considerations
Adapting heart-healthy eating to your cultural background and social situations ensures long-term adherence. Most cuisines can be modified to support cardiovascular health while maintaining familiar flavors and traditions.
Cultural Adaptation Tips:
- Identify heart-healthy traditional foods in your culture
- Modify cooking methods rather than eliminating favorite dishes
- Find healthy alternatives to high-sodium or high-fat ingredients
- Involve family members in meal planning and preparation
Monitoring Progress and Adjusting Your Approach
Key Metrics to Track
Regular monitoring helps ensure your dietary changes support your cardiovascular health goals. Work with your healthcare team to establish appropriate targets and monitoring schedules.
Important Health Markers:
- Blood pressure readings
- Cholesterol levels (total, LDL, HDL, triglycerides)
- Body weight and waist circumference
- Blood sugar levels (if diabetic or pre-diabetic)
- Overall energy and well-being
When to Seek Professional Guidance
Consider consulting with a registered dietitian or nutritionist if you experience challenges implementing dietary changes, have complex medical conditions, or need personalized meal planning assistance.
Professional Consultation Indicators:
- Difficulty managing multiple dietary restrictions
- Unclear about portion sizes or meal timing
- Struggling with meal planning or preparation
- Need help adapting cultural foods for heart health
- Experiencing unwanted weight changes
Frequently Asked Questions
What should I eat immediately after my angioplasty procedure?
Focus on light, easily digestible foods during your first few days of recovery. Choose mild options like broth-based soups, plain rice, bananas, toast, and herbal teas.
Avoid heavy, greasy, or spicy foods that might cause digestive discomfort while your body recovers from the procedure.
How soon can I return to my normal eating habits?
You can gradually transition back to a more varied diet within the first week, but this should be a heart-healthy version of your normal eating habits rather than returning to previous unhealthy patterns.
The goal is to establish new, sustainable eating habits that support your cardiovascular health long-term.
Are there any foods I need to completely eliminate forever?
Rather than complete elimination, focus on significant reduction of harmful foods. You don’t need to never eat red meat or desserts again, but these should become occasional treats rather than regular parts of your diet.
The emphasis should be on making heart-healthy foods the foundation of your eating pattern.
Can I drink alcohol after angioplasty?
Moderate alcohol consumption may be acceptable for some people, but this depends on your specific medications and overall health status.
Many heart medications interact with alcohol, and excessive alcohol can raise blood pressure and contribute to heart rhythm problems. Always discuss alcohol consumption with your healthcare provider.
How important is reducing sodium in my diet?
Sodium reduction is crucial because excess sodium increases blood pressure, which strains your cardiovascular system and can contribute to future heart problems.
Aim to consume less than 2,300 milligrams of sodium daily, or even less if your doctor recommends it. Focus on fresh foods and cook at home to better control sodium intake.
Should I take any supplements after angioplasty?
While a balanced diet should provide most necessary nutrients, some people may benefit from specific supplements like omega-3 fatty acids or vitamin D.
However, supplements can interact with heart medications, so never start any supplement regimen without discussing it with your healthcare provider first.
How can I make heart-healthy eating more affordable?
Heart-healthy eating doesn’t have to be expensive. Focus on affordable staples like beans, lentils, oats, brown rice, seasonal fruits and vegetables, and canned fish.
Buy in bulk when possible, cook at home instead of eating out, and choose frozen or canned fruits and vegetables when fresh options are too costly.
What if I have other health conditions like diabetes along with heart disease?
Multiple health conditions require coordinated nutritional management. The good news is that many dietary recommendations overlap – foods that support heart health often benefit blood sugar control as well.
Work with your healthcare team to develop an integrated approach that addresses all your health conditions simultaneously.
How do I handle social situations and dining out?
Planning ahead makes social dining easier. Review restaurant menus online beforehand, don’t hesitate to ask about preparation methods, request modifications like dressing on the side, and focus on grilled or baked options rather than fried foods.
Remember that you can enjoy social occasions while making heart-healthy choices.
Is it normal to feel overwhelmed by all these dietary changes?
Feeling overwhelmed is completely normal and common. Start with just one or two changes at a time rather than trying to overhaul your entire diet immediately.
Consider working with a registered dietitian who can help you prioritize changes and create a manageable plan that fits your lifestyle and preferences.
How will I know if my dietary changes are working?
Your healthcare provider will monitor key indicators like blood pressure, cholesterol levels, and overall cardiovascular health through regular check-ups and blood tests.
You may also notice improvements in energy levels, sleep quality, and general well-being as you consistently follow a heart-healthy eating pattern.
Can I ever eat fast food or processed foods again?
While it’s best to minimize fast food and processed foods, you don’t need to eliminate them entirely forever.
The key is making them rare exceptions rather than regular habits. When you do choose these options, look for the healthiest available choices and balance them with extra healthy foods throughout the rest of your day.
Conclusion: Your Path to Heart-Healthy Living
Recovering from angioplasty marks the beginning of a new chapter in your cardiovascular health journey. The dietary choices you make during recovery and beyond directly influence your heart’s healing process and your long-term wellness outcomes.
Remember that sustainable change happens gradually. Focus on progress rather than perfection, and celebrate each healthy choice you make.
Your commitment to heart-healthy eating, combined with appropriate medical care and lifestyle modifications, creates the foundation for a vibrant, heart-healthy future.
The investment you make in learning about and implementing these nutritional strategies pays dividends in improved quality of life, reduced risk of future cardiovascular events, and the confidence that comes from taking an active role in your health management.
Your heart has been given a second chance through angioplasty – honor that opportunity with choices that support its continued health and vitality.