Are you experiencing pain, numbness, tingling, or weakness in your arms, legs, neck, or lower back?
These symptoms may indicate that you have a herniated disc, commonly known as a slipped disc.
In this comprehensive guide, we explore what causes this often debilitating condition and the various treatment options available in Singapore.
This might help: Which Orthopedic Doctor in Singapore Should You Consider?
Understanding Slipped Discs
What is a Slipped Disc?
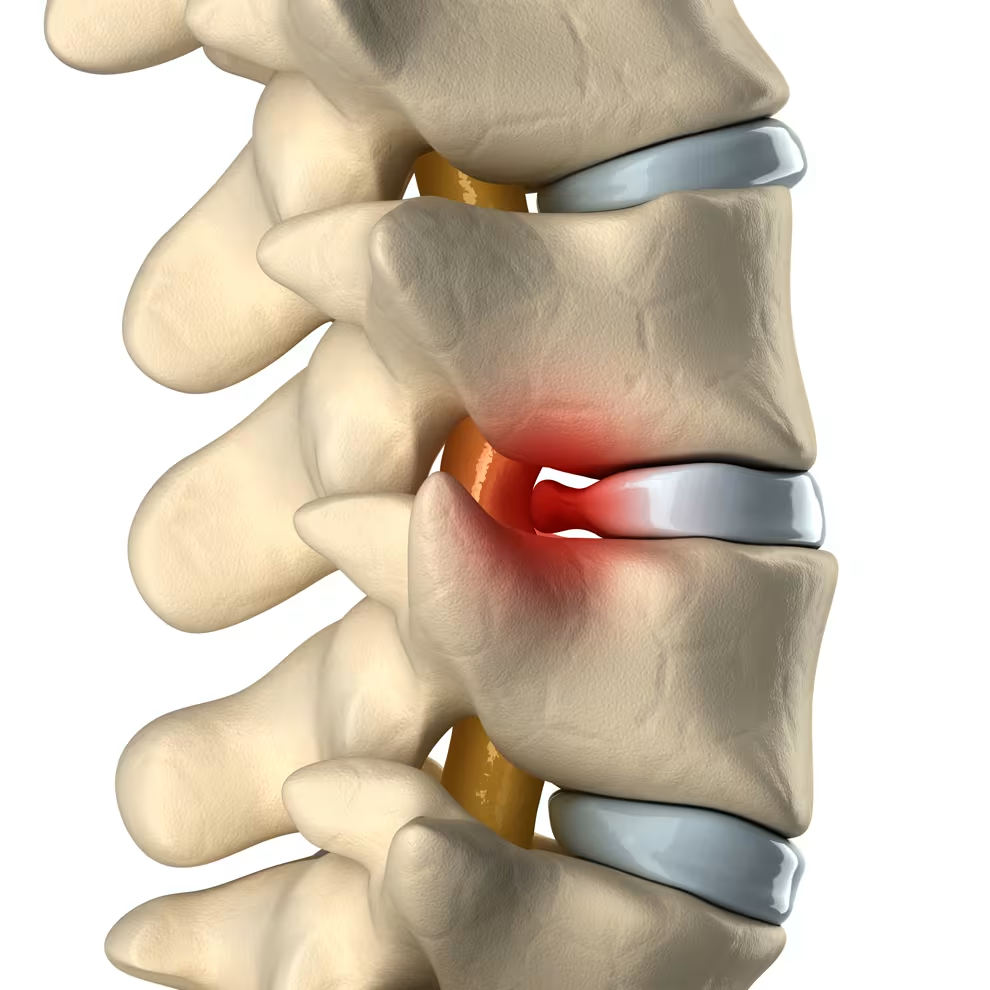
A slipped disc, medically termed as a herniated or prolapsed disc, occurs when one of the rubbery cushions (intervertebral discs) that sit between the vertebrae along your spine gets compressed and the inner gel-like material (nucleus pulposus) squeezes through the tougher outer layer (annulus fibrosus).
This protrusion can affect any disc in the entire spine and, depending on its location, may cause pain in your neck or back that radiates to your limbs, accompanied by numbness or weakness.
The structure of each intervertebral disc consists of:
- Annulus Fibrosus: The tough outer layer made of fibrocartilage that provides structure and strength.
- Nucleus Pulposus: The softer, gel-like inner core that provides cushioning and flexibility.
More information: Best Orthopedic Doctor in JB for Singaporeans
How Does a Slipped Disc Occur?
A slipped disc typically develops through a progressive series of stages that begin with structural damage to the disc’s outer layer.
The process often begins with an initial tear or small fissure in the annulus fibrosus, which usually results from mechanical stress caused by activities like heavy lifting, twisting movements, or sudden impact to the spine.
As the annulus fibrosus weakens over time, the nucleus pulposus may shift from its normal central position toward the tear in the outer layer, creating instability within the disc structure.
Eventually, the nucleus pulposus may herniate completely through the tear, causing the disc material to bulge outward beyond its normal boundaries.
The most problematic stage occurs when the protruding disc material compresses or irritates surrounding nerve structures, resulting in pain, numbness, and muscle weakness that often radiates to other parts of the body, depending on which spinal level is affected.
You might be interested: Hip Replacement Surgery in Singapore: Cost, Risks
Causes and Risk Factors
Common Causes of Slipped Discs
Slipped discs can happen to anyone, but they most commonly occur between the ages of 20-50 years when people are most active physically and occupationally.
Various factors can contribute to their development through different mechanisms.
Physical trauma from direct impact during accidents or falls can exert significant force on the spine, causing a disc to herniate immediately or creating damage that leads to herniation later.
Repetitive strain from occupations or activities involving repetitive lifting, bending, or twisting can induce chronic mechanical stress on the spine, gradually weakening the annulus fibrosus over time until it fails.
Age-related degeneration plays a significant role, as discs naturally lose water content as we age, becoming less flexible and more prone to tearing or rupturing even with minor strain.
Improper lifting techniques that involve bending at the waist rather than using the legs put excessive pressure on the lower back, while sudden movements such as twisting the back, lifting heavy objects improperly, or experiencing a fall can trigger acute disc herniation.
You might like: Tennis Elbow Treatment in Singapore: Causes, Symptoms, Recovery
Risk Factors for Disc Herniation
Beyond age, several factors can significantly increase vulnerability to experiencing a slipped disc.
Excess weight puts additional stress on the discs in the lower back, as the spine must support more load during daily activities.
Genetic predisposition may influence susceptibility to disc herniation, as family history can affect disc structure and composition.
Smoking reduces oxygen supply to the discs, accelerating their natural deterioration and making them more prone to injury.
A sedentary lifestyle involving prolonged sitting or standing in one position increases pressure on spinal discs and weakens supporting muscles.
Physically demanding occupations that require repeated lifting, bending, twisting, and pulling significantly increase risk through cumulative stress on the spine.
Poor posture during sitting or standing places uneven stress on the spine, creating areas of weakness and increased pressure.
Finally, lack of regular exercise reduces core strength, leaving the spine without adequate muscular support to protect against injury during daily activities.
Related article: Golfers Elbow Treatment in Singapore: Causes, Symptoms, Cost
Recognizing the Symptoms
Symptoms of a slipped disc typically affect one side of the body and impact the area served by the affected nerve. The presentation varies depending on the location of the herniated disc.
Lower Back (Lumbar) Disc Herniation
- Sharp or burning pain in the buttocks, thigh, or calf
- Pain that worsens when sitting, standing, coughing, or sneezing
- Numbness or tingling along the affected leg
- Muscle weakness in the same leg, potentially affecting walking ability
- Pain that increases during certain activities like bending forward
Neck (Cervical) Disc Herniation
- Pain in the shoulder and arm area
- Neck pain that may worsen with movement
- Radiating pain down to the fingers
- Numbness or tingling in the arm, shoulder, or hand
- Weakness in the affected arm or hand
You might be interested: Scoliosis Treatment in Singapore: Causes and Symptoms
Warning Signs Requiring Immediate Medical Attention
Certain symptoms associated with disc herniation require immediate medical evaluation as they may indicate serious complications that could result in permanent damage if left untreated.
You should seek medical treatment without delay if your symptoms progressively worsen despite conservative treatment measures, or if you experience difficulty urinating, which may indicate nerve compression affecting bladder function.
Loss of control over bladder or bowel function represents a medical emergency that requires immediate intervention to prevent permanent nerve damage.
Similarly, you should seek urgent care if you notice loss of sensation in the inner thighs, back of legs, or around the rectum, as this pattern suggests compression of critical nerve pathways.
Severe, unmanageable pain that does not respond to standard pain relief measures may indicate significant nerve compression or other serious complications.
Additionally, if you develop weakness that interferes with normal daily activities such as walking, climbing stairs, or lifting objects, prompt medical evaluation is essential to prevent further deterioration.
Read more: Low Back Pain in Singapore: Causes, Prevention and Treatment
Diagnosing a Slipped Disc in Singapore
Proper diagnosis is essential for appropriate treatment. In Singapore, orthopedic specialists employ several approaches to identify and evaluate slipped discs.
Physical Examination
During an initial consultation for suspected disc herniation, your doctor will conduct a comprehensive evaluation to assess the extent and location of your condition.
The examination begins with a careful physical assessment focused on the affected spinal area, including observation of your posture and spinal curvature to identify any obvious deformities or compensatory changes.
Your doctor will assess your ability to perform specific movements such as bending forward, backward, and to the sides to determine which motions trigger or worsen your symptoms.
The examination includes checking for areas of numbness or loss of sensation by testing your response to light touch and pinprick sensations in various locations.
Muscle reflexes and strength are evaluated systematically to identify any neurological deficits that might indicate nerve compression or damage.
For suspected lumbar disc herniation, doctors often perform specific diagnostic tests like the straight leg raise test, which can help confirm the diagnosis and identify the affected spinal level.
Diagnostic Tests
To confirm the diagnosis and determine the precise location and severity of disc herniation, your physician may order:
- Magnetic Resonance Imaging (MRI): The gold standard for diagnosing slipped discs, providing detailed images of both bone and soft tissues
- Computerized Tomography (CT) Scan: Creates cross-sectional images of the spinal column and surrounding structures
- X-Rays: Helps rule out other conditions like fractures or spinal deformities
- Electromyography (EMG): Evaluates electrical activity in muscles and helps determine the exact nerve root involved
- Nerve Conduction Studies: Measures electrical impulses in nerve signals
- Myelogram: Uses dye injected around the spinal cord to identify areas of pressure
Non-Surgical Treatment Options in Singapore
Most people with a herniated disc don’t require surgery. In Singapore, the standard approach follows a conservative treatment path before considering surgical intervention. About 90% of patients respond well to non-surgical treatments within 6-8 weeks.
Rest and Modified Activity
- Short-term rest (1-2 days) to reduce acute pain
- Gradual return to regular activities while avoiding movements that exacerbate symptoms
- Modification of activities to prevent strain on your back
- Avoiding heavy lifting and maintaining good posture
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in recovery and typically includes:
- Specific exercises to strengthen core muscles
- Stretching techniques to improve flexibility
- McKenzie Back Extension exercises for lumbar disc herniations
- Education on proper body mechanics and posture
- Heat or cold therapy to manage pain
- Ultrasound, electrical stimulation, or massage therapy
- Traction for cervical disc herniations
Pain Management
Various medication options can help control pain and inflammation:
- Over-the-counter analgesics: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen
- Muscle relaxants: To relieve muscle spasms associated with disc herniation
- Prescription pain medications: For short-term use in cases of severe pain
- Nerve pain medications: Drugs such as gabapentin, pregabalin, duloxetine, tramadol, and amitriptyline to address nerve-related pain
Corticosteroid Injections
When oral medications prove insufficient for managing disc-related pain and inflammation, your doctor may recommend more targeted injection therapy.
Epidural steroid injections deliver anti-inflammatory medication directly around the affected spinal nerves, providing more concentrated treatment at the source of the problem.
These injections are performed using spinal imaging guidance such as fluoroscopy or CT scanning to ensure precise needle placement and maximize therapeutic effectiveness while minimizing risks.
The steroid medication can provide temporary but significant relief that may last for weeks or months, allowing sufficient time for natural healing processes to occur and potentially avoiding the need for surgical intervention.
Percutaneous Disc Nucleoplasty
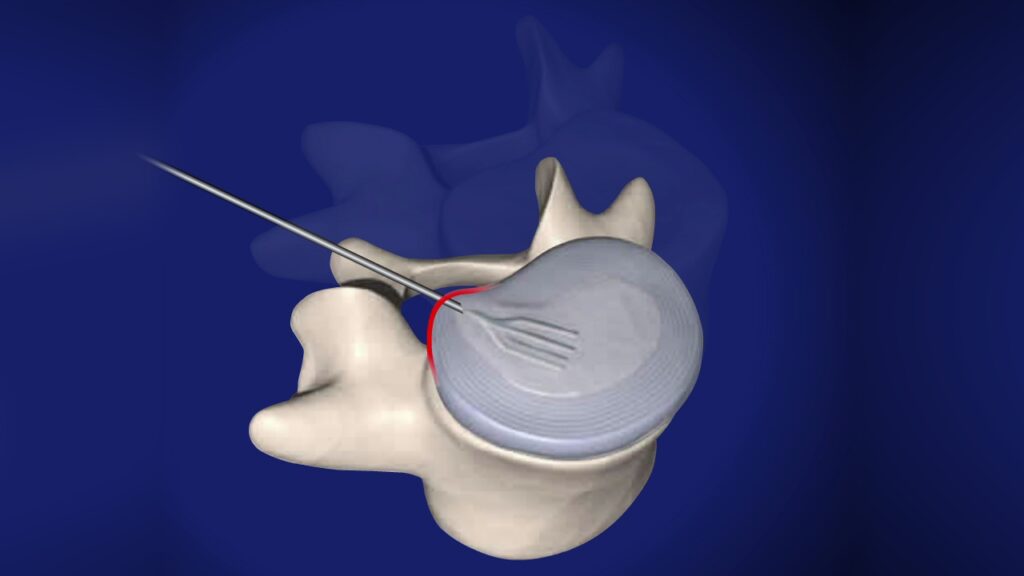
This minimally invasive procedure represents an advanced treatment option available in Singapore for patients who have not responded adequately to conservative treatments such as medications, physical therapy, and injections.
The procedure involves inserting a small needle directly into the problematic intervertebral disc to decompress it without requiring any surgical incision.
Percutaneous disc nucleoplasty is typically performed as a 20-minute outpatient procedure under local anesthesia in a day surgery setting, allowing patients to return home the same day.
Most patients can walk almost immediately after the procedure with minimal downtime compared to traditional surgical approaches.
The treatment works by reducing pressure within the disc, which alleviates pain symptoms and may allow the disc to return toward its normal position.
Surgical Treatment Options in Singapore
When conservative treatments fail to provide relief after 6-8 weeks, or if neurological symptoms worsen, surgical intervention may be necessary. Singapore offers several advanced surgical options for treating slipped discs.
When Surgery Becomes Necessary
Surgery may be recommended if:
- There’s evidence of severe nerve compression
- Symptoms haven’t improved with non-surgical treatments
- You experience difficulty standing or walking
- You show signs of progressive muscle weakness
- You develop altered bladder or bowel function
- Your quality of life is significantly affected by persistent pain
Types of Surgical Procedures
Discectomy/Microdiscectomy
The most common surgical procedure for herniated discs in the lumbar spine:
- Removal of the portion of the disc that’s pressing on nerve roots
- May be performed through a small incision using microscopic visualization (microdiscectomy)
- Usually requires a brief hospital stay for observation
- High success rate for appropriate candidates
Laminotomy/Laminectomy
- Creates more space for nerves by removing a small window in the vertebral arch (lamina)
- Laminectomy involves removing the entire lamina
- Often performed in conjunction with discectomy
- Useful when broader decompression is needed
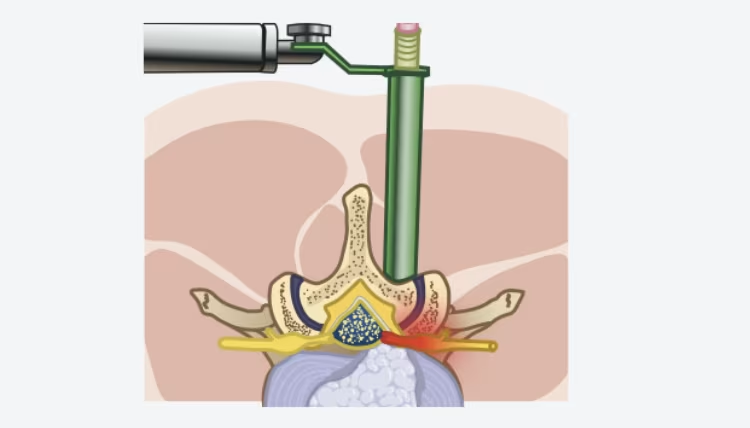
Endoscopic Discectomy
A minimally invasive option available in Singapore:
- Uses an endoscope (a thin tube with a camera) inserted through a small incision
- Allows the surgeon to visualize and remove the herniated disc material
- Typically performed as outpatient surgery
- Offers faster recovery times than traditional open procedures
Artificial Disc Replacement
- Replaces the damaged disc with an artificial one made of plastic or metal
- Performed under general anesthesia through an incision in the abdomen or neck
- Suitable primarily for single-level disc herniation in patients without arthritis or osteoporosis
- Preserves motion at the affected spinal segment
Spinal Fusion
- Permanently connects two or more vertebrae using bone grafts and metal hardware
- Eliminates motion between the fused vertebrae
- Necessary when there’s significant instability or when other procedures aren’t suitable
- Requires longer recovery and rehabilitation
Surgery on the Core of the Spinal Disc
- Uses vacuum technology to remove the core of the spinal disc
- Reduces the size of the disc to relieve pressure on nearby nerves
- Can only be performed if the outer layer of the disc remains intact
- Less invasive than complete disc removal
Recovery and Rehabilitation
Recovery following slipped disc treatment varies based on the approach and individual factors. Here’s what to expect:
After Non-Surgical Treatment
- Most patients see improvement within 4-6 weeks of consistent conservative care
- Physical therapy continues to strengthen supporting muscles
- Gradual return to regular activities with modified techniques
- Ongoing attention to proper body mechanics and posture
Post-Surgical Recovery
Recovery timelines depend on the procedure:
- Discectomy/Microdiscectomy: Return to light activities within 2-6 weeks
- Laminectomy: Recovery typically takes 4-8 weeks
- Endoscopic Procedures: Often allows return to normal activities within 2-4 weeks
- Artificial Disc Replacement: Hospital stay of a few days with gradual activity resumption
- Spinal Fusion: Longer recovery period, ranging from 3-6 months
Your surgeon will provide specific instructions regarding:
- Activity restrictions during recovery
- Appropriate exercises for rehabilitation
- When to resume normal activities
- Follow-up appointments to monitor healing
Preventing Slipped Discs
While not all disc herniations can be completely prevented, particularly those related to genetic factors or normal aging, several evidence-based strategies can significantly reduce your risk of developing this condition.
Maintain Proper Posture
Maintaining proper spinal alignment during daily activities is fundamental to disc health and injury prevention.
Keep your back straight when sitting and standing, avoiding slouched or twisted positions that place uneven stress on spinal structures.
Using ergonomic furniture at work and home helps support natural spinal curves and reduces strain during prolonged activities.
Taking regular breaks from prolonged sitting allows discs to decompress and prevents the buildup of pressure that occurs with sustained positioning.
Positioning computer screens at eye level prevents the forward head posture that can strain cervical discs and create compensatory stress throughout the spine.
Exercise Regularly
A comprehensive exercise program targeting core muscle strength provides essential support for spinal structures and reduces the risk of disc injury.
Improving flexibility through regular stretching helps maintain normal range of motion and prevents the muscle tightness that can contribute to spinal dysfunction.
Engaging in low-impact aerobic activities such as walking, swimming, or cycling promotes disc nutrition through improved circulation while avoiding high-impact stresses that might damage weakened discs.
Many individuals benefit from working with a physical therapist who can provide personalized guidance on exercise selection and proper technique.
Practice Safe Lifting Techniques
Proper lifting mechanics are crucial for preventing acute disc herniation during daily activities.
Always bend at the knees rather than at the waist when lifting objects, as this technique utilizes the powerful leg muscles while maintaining proper spinal alignment.
Keep objects as close to your body as possible during lifting to minimize the leverage forces acting on your spine.
Avoid twisting movements while lifting or carrying heavy items, as rotational forces combined with compression can easily exceed the disc’s capacity to withstand stress.
For very heavy items, always seek assistance rather than attempting to lift alone, regardless of your physical condition or experience.
Maintain a Healthy Weight
Excess body weight places additional strain on spinal structures, particularly the discs in the lower back that bear the greatest load during daily activities.
Following a balanced diet combined with a regular exercise regimen helps achieve and maintain optimal body weight while providing additional benefits for overall spinal health.
Avoid Smoking
Smoking significantly reduces the delivery of oxygen and nutrients to spinal discs, accelerating their natural degeneration process and making them more susceptible to injury.
The chemicals in tobacco also interfere with the body’s ability to repair damaged tissues, prolonging recovery times when injuries do occur.
If you currently smoke, seeking professional support for smoking cessation represents one of the most important steps you can take to protect your spinal health.
When to Consult an Orthopedic Specialist in Singapore
If you’re experiencing symptoms that suggest a slipped disc, don’t delay seeking medical advice. Consult an orthopedic specialist in Singapore if:
- Back or neck pain persists for more than a week
- Pain radiates down your arm or leg
- You experience numbness, tingling, or weakness in limbs
- Pain interferes with daily activities or sleep
- You’ve recently experienced trauma to your back or neck
- You develop any bladder or bowel control issues
Early intervention can prevent worsening of the condition and improve treatment outcomes.
Frequently Asked Questions
What is the difference between a bulging disc and a slipped disc?
A bulging disc occurs when the disc extends beyond its normal boundaries but maintains its structural integrity.
It typically affects a larger portion of the disc’s circumference (around 25-50%) and is often related to age-related degeneration.
In contrast, a slipped disc (herniated disc) involves an actual tear in the tough outer layer of the disc, allowing the soft inner material to leak into the spinal canal.
Slipped discs usually affect a smaller, more localized area and tend to cause more significant pain as they’re more likely to compress nearby nerves.
How long does it take to recover from a slipped disc without surgery?
Most patients with a slipped disc who follow conservative treatment recommendations experience significant improvement within 4-6 weeks.
Complete recovery without surgery typically occurs within 6-12 weeks, though this varies based on the severity of the herniation, your overall health, and your adherence to treatment protocols.
Some patients notice improvement within days of beginning appropriate rest and medication, while others may take longer to experience relief.
Can a slipped disc heal on its own?
Yes, many slipped discs can heal on their own with proper conservative management.
The body has natural healing mechanisms that can gradually reabsorb the herniated disc material over time. This process typically takes several weeks to months.
During this healing period, conservative treatments like rest, physical therapy, and pain management can help control symptoms and facilitate recovery.
However, severely herniated discs or those causing significant nerve compression may require more aggressive interventions.
Will I need surgery for my slipped disc?
Most patients with slipped discs, approximately 90%, do not require surgical intervention.
Conservative treatments including rest, physical therapy, pain medication, and steroid injections are typically effective in managing symptoms and promoting natural healing processes.
Surgery is generally considered only when conservative treatments have failed after 6-8 weeks of consistent application, when patients experience progressive neurological deficits such as worsening numbness or weakness, when there is loss of bladder or bowel control, or when pain remains severe and unmanageable with other treatment approaches.
Your doctor will thoroughly evaluate your specific condition before recommending any surgical intervention.
What activities should I avoid with a slipped disc?
When managing a slipped disc, it’s important to avoid activities that place additional stress on your spine.
These include heavy lifting of anything over 5 kilograms, prolonged sitting or standing in one position, bending forward at the waist, and twisting motions of the spine.
High-impact exercises like running or jumping should be avoided, along with sports involving sudden directional changes and any activities that worsen your pain symptoms.
Your physical therapist can provide personalized guidance about which activities are safe based on your specific condition and current recovery stage.
Can physiotherapy cure a slipped disc?
While physiotherapy cannot “cure” a slipped disc in the sense of immediately repairing the herniation, it plays a crucial role in recovery by reducing pain and inflammation, improving spinal mobility, strengthening supporting muscles, teaching proper body mechanics to prevent further injury, and facilitating the body’s natural healing process.
A comprehensive physiotherapy program tailored to your specific condition can significantly improve symptoms and function, potentially eliminating the need for more invasive treatments like surgery.
Is swimming good for slipped disc recovery?
Swimming and water-based exercises are generally excellent for slipped disc recovery because the buoyancy of water reduces pressure on the spine, provides gentle resistance for muscle strengthening, allows for movement with minimal pain, and improves cardiovascular fitness without jarring impacts.
Always consult with your healthcare provider before beginning any exercise program, and consider working with a physical therapist who can recommend specific water exercises appropriate for your condition.
How long should I rest with a slipped disc?
Contrary to traditional advice, prolonged bed rest is not recommended for slipped disc recovery.
Current medical guidelines suggest limiting bed rest to 1-2 days at most. After this initial period, gradually returning to normal activities within pain limits is beneficial.
Too much rest can lead to muscle weakness, stiffness, and potentially slower recovery. Instead, focus on modified activities that don’t exacerbate your symptoms, while avoiding those that increase pain.
Can stress make a slipped disc worse?
Stress can potentially worsen slipped disc symptoms through several mechanisms including increased muscle tension around the spine, heightened pain perception, poor sleep quality affecting recovery, stress-related inflammation in the body, and less attention to proper body mechanics when stressed.
Incorporating stress management techniques like deep breathing, meditation, progressive muscle relaxation, and adequate sleep into your recovery plan can help minimize these negative effects.
What is the success rate of slipped disc surgery in Singapore?
The success rate for slipped disc surgery in Singapore is generally high, with approximately 80-90% of patients experiencing significant pain relief and improved function following appropriate surgical intervention.
Factors affecting success include the type of surgical procedure performed, severity and location of the disc herniation, patient’s overall health and adherence to post-operative recommendations, and presence of other spinal conditions.
Modern surgical techniques and advanced medical facilities in Singapore contribute to these favorable outcomes for properly selected surgical candidates.
Will I have permanent damage from a slipped disc?
Most patients with slipped discs recover completely without permanent damage, especially with prompt and appropriate treatment.
However, prolonged nerve compression can potentially lead to permanent issues such as persistent numbness or weakness, chronic pain, altered sensation in affected areas, or cauda equina syndrome in severe cases.
The risk of permanent damage increases with the severity of herniation, duration of nerve compression, and delayed treatment.
Early intervention significantly reduces this risk, highlighting the importance of seeking medical attention promptly when symptoms develop.
Can I drive with a slipped disc?
Driving with a slipped disc depends on several factors including the severity of your symptoms, your ability to maintain proper posture, whether your medication causes drowsiness, your capacity to react quickly if needed, and the location of your herniated disc.
Cervical herniations may limit neck mobility needed for checking blind spots, while lumbar herniations may affect sitting tolerance.
For many patients with mild to moderate symptoms, short drives may be tolerable with proper seat adjustments and lumbar support, though you should consult your healthcare provider for personalized advice.
What are the best sleeping positions for someone with a slipped disc?
Optimal sleeping positions for slipped disc patients depend Optimal sleeping positions for slipped disc patients depend on the herniation location.
For lumbar disc herniations, side sleeping with knees bent and a pillow between the knees is recommended, along with back sleeping with a pillow under the knees to maintain the spine’s natural curve. Stomach sleeping should be avoided as it increases lumbar lordosis and stress on the discs.
For cervical disc herniations, back sleeping with a specialized cervical pillow that supports the neck’s natural curve is preferred, along with side sleeping using proper pillow height to maintain neck alignment.
Stomach sleeping should be avoided as it twists the neck unnaturally. Regardless of position, using a medium-firm mattress that provides adequate support without excessive sinking is recommended for all patients.

