Insomnia affects millions worldwide, and Singapore is no exception. This sleep disorder, characterized by persistent difficulties in falling asleep, staying asleep, or achieving restorative sleep, can significantly impact your daily life, work performance, and overall well-being.
Understanding the various treatment options available in Singapore is crucial for anyone struggling with sleep difficulties.
This comprehensive guide explores everything you need to know about insomnia treatment in Singapore, from understanding the condition to accessing the most effective therapeutic interventions available in the city-state.
Related article: Which Psychologist in Singapore Should You Consider? (Sort by Reviews)
Understanding Insomnia: More Than Just Sleepless Nights

Insomnia represents a complex sleep disorder that extends far beyond occasional restless nights. When sleep difficulties persist and begin interfering with your daytime functioning, they may qualify as Insomnia Disorder.
This condition requires adequate sleep opportunity but still results in significant distress or impairment in social, occupational, educational, or behavioral aspects of life.
The impact of untreated insomnia extends beyond mere fatigue. Research consistently demonstrates associations with psychiatric and physical health complications, reduced quality of life, increased accident risks, and substantial healthcare costs.
Understanding these broader implications underscores the importance of seeking appropriate treatment.
You might like: Which Psychiatrist in Singapore Should You Consider?
Types of Insomnia: Identifying Your Sleep Pattern
Primary vs Secondary Classification
Primary Insomnia occurs independently without direct connections to other medical, psychiatric, or substance-related conditions. This type often develops through psychological conditioning where individuals begin associating their bed or bedroom with stress and sleeplessness, creating a self-perpetuating cycle.
Secondary (Comorbid) Insomnia represents the more common form, arising from or being aggravated by underlying medical conditions, psychiatric disorders, or substance use.
Identifying secondary insomnia involves examining whether sleep difficulties follow the course of another condition or improve when the primary condition is treated.
Related article: Eating Disorder Treatment in Singapore: Causes, Recovery
Duration-Based Categories
| Type | Duration | Characteristics |
|---|---|---|
| Episodic Insomnia | 1-3 months | Short-term difficulties often related to stress or life changes |
| Persistent (Chronic) Insomnia | 3+ months | Long-term sleep difficulties requiring comprehensive intervention |
| Recurrent Insomnia | Multiple episodes within a year | Repeated 1-3 month periods of sleep difficulties |
Specific Insomnia Subtypes
Sleep-Onset Insomnia involves difficulty initiating sleep, with individuals spending extended periods trying to fall asleep despite feeling tired.
This type particularly affects those with early morning responsibilities.
Sleep-Maintenance Insomnia characterized by frequent nighttime awakenings with difficulty returning to sleep. Individuals typically wake multiple times and struggle for extended periods before falling back asleep.
Mixed Insomnia combines both onset and maintenance difficulties, presenting the most complex treatment challenges.
Paradoxical Insomnia involves perceived sleep deprivation despite adequate sleep duration as measured in sleep studies, often resulting from heightened awareness during sleep periods.
You might like: Anxiety Therapy in Singapore: Treatment and Recovery
Recognizing Insomnia Symptoms and Diagnostic Criteria
Primary Symptoms
The hallmark symptoms of insomnia extend beyond nighttime sleep difficulties to encompass significant daytime impairments:
- Persistent difficulty falling asleep despite fatigue
- Frequent nighttime awakenings with prolonged periods of wakefulness
- Early morning awakenings with inability to return to sleep
- Chronic daytime fatigue and excessive sleepiness
- Cognitive impairments including concentration difficulties and memory problems
- Mood disturbances such as irritability, anxiety, or depression
- Decreased performance in work, academic, or social settings
- Physical symptoms including headaches and gastrointestinal issues
This might help: PTSD Treatment in Singapore: Types, Recovery and Healing
Diagnostic Criteria
Healthcare professionals in Singapore utilize established diagnostic criteria to identify Insomnia Disorder:
- Sleep Quality Complaints: Documented dissatisfaction with sleep quantity or quality
- Frequency Requirements: Sleep difficulties occurring at least three nights per week
- Duration Criteria: Symptoms persisting for minimum three months
- Functional Impact: Demonstrable impairment in daily functioning across multiple life domains
- Opportunity Assessment: Adequate sleep opportunity and environment
- Differential Diagnosis: Exclusion of other sleep-wake disorders or substance effects
Read more: Psychotherapy in Singapore: Types, Benefits, and How to Get Started
Comprehensive Causes and Risk Factors
Psychological and Psychiatric Factors
Mental health conditions represent primary contributors to insomnia development. Anxiety disorders create hypervigilance that interferes with the natural sleep transition.
Depression frequently disrupts sleep architecture, leading to early morning awakenings and reduced sleep quality.
Post-traumatic stress disorder (PTSD) can trigger nightmares and hyperarousal states that severely impact sleep.
Chronic stress from work pressures, financial concerns, relationship difficulties, or major life transitions activates the body’s stress response system, maintaining alertness when sleep should occur.
Physical and Medical Conditions
Numerous medical conditions contribute to insomnia through pain, discomfort, or physiological disruption:
- Respiratory Conditions: Asthma, sleep apnea, and chronic obstructive pulmonary disease
- Cardiovascular Issues: Heart disease, arrhythmias, and hypertension
- Neurological Disorders: Alzheimer’s disease, Parkinson’s disease, and seizure disorders
- Chronic Pain Conditions: Arthritis, fibromyalgia, and back problems
- Endocrine Disorders: Hyperthyroidism, diabetes, and hormonal imbalances
- Gastrointestinal Problems: Gastroesophageal reflux disease (GERD) and irritable bowel syndrome
Related article: Complete Guide to Depression Therapy in Singapore
Lifestyle and Environmental Factors
Modern lifestyle patterns significantly impact sleep quality. Excessive caffeine consumption, particularly in afternoon or evening hours, maintains alertness well into intended sleep periods.
Alcohol consumption, while initially sedating, disrupts sleep architecture and leads to fragmented rest.
Irregular sleep schedules due to shift work, frequent travel, or inconsistent bedtime routines disrupt circadian rhythms.
Environmental factors including noise pollution, excessive light exposure, uncomfortable temperatures, and poor bedding quality create additional barriers to quality sleep.
Screen time exposure, particularly blue light from electronic devices, suppresses melatonin production and delays sleep onset.
The stimulating content consumed through digital media can also maintain mental arousal when relaxation should occur.
Age and Gender Considerations
Research indicates that individuals over 60 experience increased insomnia susceptibility due to natural changes in sleep architecture, including reduced deep sleep and REM periods.
Women face higher insomnia rates, particularly during hormonal transition periods such as menstruation, pregnancy, and menopause.
Evidence-Based Treatment Approaches in Singapore
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I represents the gold standard first-line treatment for chronic insomnia, widely available through Singapore’s healthcare system.
This structured approach typically involves 6-8 sessions lasting 30-60 minutes each, focusing on identifying and modifying thoughts and behaviors that perpetuate sleep difficulties.
Cognitive Components address maladaptive beliefs about sleep, catastrophic thinking about sleep loss consequences, and performance anxiety related to sleep.
Patients learn to challenge unrealistic sleep expectations and develop more balanced perspectives about sleep variability.
Behavioral Interventions include multiple evidence-based techniques:
Sleep Restriction Therapy initially limits time spent in bed to match actual sleep time, creating mild sleep deprivation that promotes faster sleep onset and improved sleep efficiency. Bedtime is gradually extended as sleep quality improves.
Stimulus Control Therapy re-establishes the bedroom and bed as cues for sleep rather than wakefulness.
This involves using the bed only for sleep, leaving the bedroom when unable to sleep within 15-20 minutes, and maintaining consistent wake times regardless of sleep duration.
Relaxation Training encompasses progressive muscle relaxation, deep breathing exercises, mindfulness meditation, and guided imagery techniques that activate the parasympathetic nervous system and facilitate the transition to sleep.
Pharmacological Interventions
Prescription Medications available in Singapore include several categories:
Benzodiazepines provide effective short-term relief but carry risks of dependence, tolerance, and daytime sedation. These medications are typically reserved for brief treatment periods during acute sleep crises.
Non-Benzodiazepine Hypnotics (Z-drugs) such as zolpidem, eszopiclone, and zaleplon offer improved safety profiles with reduced dependence risk while maintaining efficacy for sleep initiation.
Melatonin Receptor Agonists work by enhancing the body’s natural sleep-wake regulation, particularly effective for circadian rhythm disorders and jet lag recovery.
Off-Label Medications including certain antidepressants and antihistamines may be prescribed when primary sleep medications are unsuitable or when treating comorbid conditions.
Advanced Medical Interventions
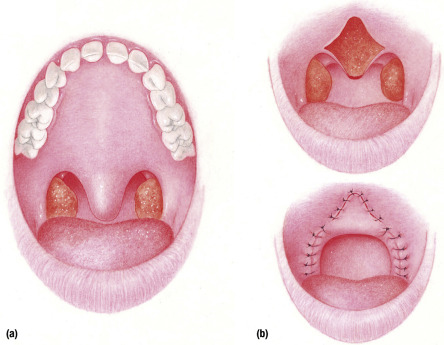
For severe cases involving obstructive sleep apnea or structural abnormalities, surgical options available in Singapore include:
Uvulopalatopharyngoplasty (UPPP) removes excess throat tissue to improve airway patency during sleep.
Maxillomandibular Advancement surgically repositions jaw structures to enlarge upper airway dimensions.
Hypoglossal Nerve Stimulation represents an innovative approach using implanted devices to prevent tongue-based airway obstruction.
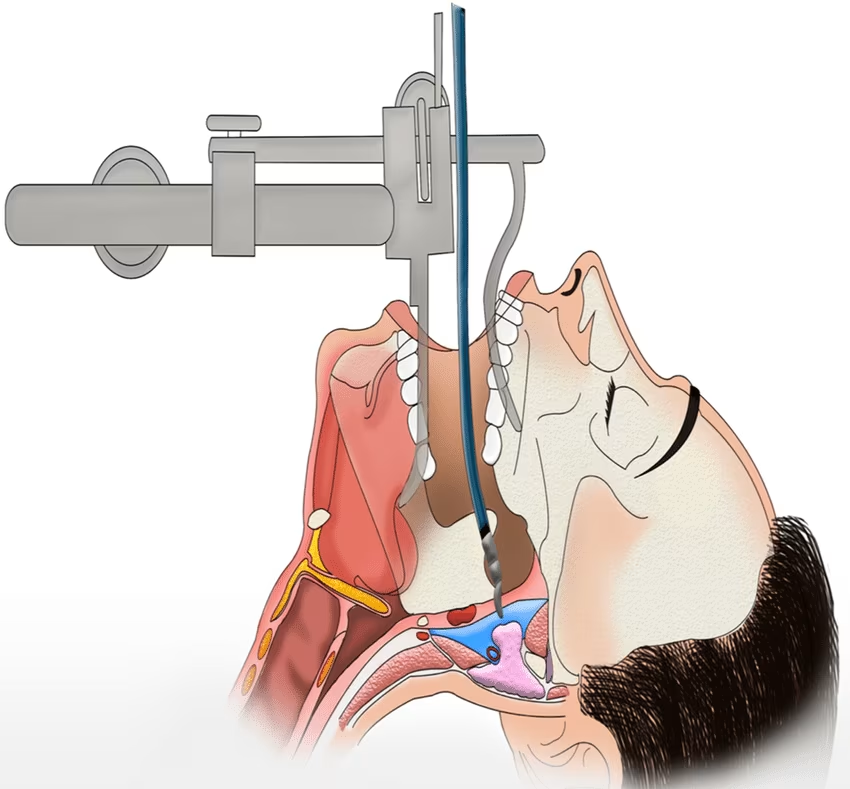
Transoral Robotic Surgery (TORS) offers minimally invasive treatment for tongue base obstructions using advanced robotic systems.
Sleep Hygiene and Lifestyle Modifications
Environmental Optimization
Creating an optimal sleep environment forms the foundation of effective insomnia treatment.
Bedrooms should maintain temperatures between 15.5-19.5°C, as cooler environments facilitate the natural temperature drop that signals sleep onset.
Light management requires eliminating or minimizing artificial light sources, particularly blue light from electronic devices.
Blackout curtains, eye masks, or light-filtering window treatments can significantly improve sleep quality.
Noise control involves identifying and addressing sound sources that disrupt sleep. White noise machines, earplugs, or sound-dampening materials can create more conducive sleep environments.
Dietary and Substance Considerations
Timing and content of food and beverage consumption significantly impact sleep quality. Large meals within three hours of bedtime can cause discomfort and interfere with sleep onset.
Spicy, acidic, or high-fat foods may trigger gastroesophageal reflux that disrupts sleep.
Caffeine consumption should be limited after 2 PM, as this stimulant can remain active in the system for 6-8 hours.
Individual sensitivity varies, and some people may need to avoid caffeine entirely after noon.
Alcohol consumption requires careful consideration. While alcohol may initially promote drowsiness, it significantly disrupts sleep architecture, reduces REM sleep, and increases nighttime awakenings as it metabolizes.
Exercise and Physical Activity
Regular physical activity improves sleep quality through multiple mechanisms, including stress reduction, body temperature regulation, and circadian rhythm reinforcement.
However, vigorous exercise within four hours of bedtime can be stimulating and should be avoided.
Morning or afternoon exercise exposure to natural light helps maintain healthy circadian rhythms and promotes alertness during appropriate daytime hours.
Understanding Costs and Insurance Coverage in Singapore
Treatment Cost Overview
| Treatment Type | Cost Range (SGD) | Duration/Sessions |
|---|---|---|
| CBT-I | $150 – $250 | Per session (6-8 sessions typical) |
| Sleep Study | $1,500 – $2,500 | Single overnight study |
| Medication Consultation | $100 – $200 | Per consultation |
| Light Therapy | $80 – $150 | Per session |
| UPPP Surgery | $5,000 – $15,000 | One-time procedure |
| Maxillomandibular Advancement | $20,000 – $40,000 | One-time procedure |
| Hypoglossal Nerve Stimulation | $30,000 – $50,000 | One-time procedure |
Insurance and Medisave Coverage
Singapore citizens and permanent residents can utilize Medisave accounts for approved sleep-related treatments, subject to annual limits and approved procedures.
Many private insurance plans provide coverage for sleep disorder treatments, with variations in coverage limits and approved providers.
Integrated Shield Plans offer enhanced coverage options:
- AIA HealthShield Gold Max A
- NTUC Income Enhanced IncomeShield Preferred
- Great Eastern HealthConnect
Employer-provided insurance plans may include direct billing arrangements with sleep clinics, reducing out-of-pocket expenses for employees.
Accessing Subsidized Care
Public healthcare institutions in Singapore offer subsidized rates for citizens and permanent residents seeking insomnia treatment.
Polyclinics provide initial assessment and referral services, while public hospitals offer specialized sleep medicine services at subsidized rates.
Community Health Assist Scheme (CHAS) provides additional subsidies for lower-income individuals seeking outpatient treatments, including some sleep-related interventions.
Prevention Strategies and Long-Term Management
Establishing Healthy Sleep Habits
Consistent sleep scheduling forms the cornerstone of insomnia prevention. Going to bed and waking at the same times daily, including weekends, helps regulate circadian rhythms and improve sleep quality over time.
Pre-sleep routines signal the body to prepare for rest. These routines should begin 30-60 minutes before intended sleep time and include calming activities such as reading, gentle stretching, or meditation.
Stress Management and Mental Health
Developing effective stress management techniques prevents stress-related insomnia development. Regular mindfulness practice, journaling, or engaging in hobbies can provide emotional outlets and reduce bedtime rumination.
Addressing underlying mental health conditions through appropriate treatment prevents secondary insomnia development and improves overall sleep quality.
Technology and Sleep Hygiene
Establishing digital boundaries involves creating device-free zones in bedrooms and implementing “digital sunsets” where electronic device use ends at least one hour before bedtime.
Blue light filtering applications or glasses can reduce the circadian rhythm disruption caused by evening screen exposure when complete avoidance isn’t possible.
When to Seek Professional Help
Warning Signs Requiring Medical Attention
Certain symptoms indicate the need for immediate professional evaluation:
- Sleep difficulties persisting beyond several weeks despite self-help efforts
- Significant daytime impairment affecting work, relationships, or safety
- Depression, anxiety, or other mental health symptoms accompanying sleep problems
- Microsleep episodes during daily activities, particularly while driving
- Loud snoring with breathing interruptions observed by sleep partners
- Excessive daytime sleepiness despite adequate sleep opportunity
Choosing the Right Healthcare Provider
Primary care physicians can provide initial assessment and treatment for mild to moderate insomnia.
For complex cases or treatment-resistant insomnia, referral to sleep medicine specialists ensures access to comprehensive diagnostic tools and advanced treatment options.
Psychologists specializing in sleep disorders offer CBT-I and other behavioral interventions, while psychiatrists can address comorbid mental health conditions requiring medication management.
Frequently Asked Questions
How long does it typically take to see improvement with insomnia treatment?
Most people begin experiencing improvements within 2-4 weeks of starting treatment, though full benefits from CBT-I may take 6-8 weeks to develop completely.
Medications often provide more immediate relief but should be combined with behavioral approaches for lasting results.
Can insomnia treatment be effective for elderly patients in Singapore?
Yes, insomnia treatment remains highly effective for elderly patients, though approaches may be modified to account for age-related factors such as medical comorbidities and medication interactions.
CBT-I is particularly valuable for older adults as it avoids potential medication complications.
What role does Traditional Chinese Medicine play in insomnia treatment in Singapore?
Traditional Chinese Medicine (TCM) is widely available in Singapore and many practitioners integrate acupuncture, herbal treatments, and lifestyle counseling for insomnia management. Some patients find combining TCM with conventional treatments provides enhanced benefits, though scientific evidence varies by specific intervention.
Are there specialized insomnia treatment centers in Singapore?
Singapore offers several specialized sleep centers within public hospitals like Singapore General Hospital and National University Hospital, as well as private facilities.
These centers provide comprehensive sleep studies, specialized treatments, and multidisciplinary care teams.
How effective is online or telemedicine-based insomnia treatment?
Digital CBT-I programs and telemedicine consultations have shown comparable effectiveness to in-person treatment for many patients.
Singapore’s healthcare system increasingly incorporates digital health solutions, making these options more accessible for individuals with scheduling constraints or mobility limitations.
What should I expect during a sleep study in Singapore?
Sleep studies typically involve overnight monitoring at a specialized facility where technicians monitor brain waves, breathing patterns, heart rate, and movement. The process is generally comfortable, with private rooms designed to simulate home sleeping environments while allowing comprehensive data collection.
Can workplace factors contribute to insomnia, and how can they be addressed?
Workplace stress, irregular schedules, and excessive screen time commonly contribute to insomnia development.
Addressing these factors may involve workplace accommodations, stress management programs, and ergonomic improvements to reduce physical discomfort that interferes with sleep.
How does Singapore’s climate affect sleep quality and insomnia treatment?
Singapore’s tropical climate and high humidity can impact sleep quality, making environmental modifications particularly important.
Air conditioning, appropriate bedding materials, and humidity control become essential components of comprehensive insomnia treatment in this climate.
Are there specific considerations for treating insomnia in shift workers in Singapore?
Shift work sleep disorder requires specialized approaches including strategic light exposure, melatonin timing, and modified sleep scheduling.
Singapore’s 24-hour economy means many healthcare providers have experience treating shift work-related sleep issues.
What alternatives exist if first-line treatments don’t work?
Treatment-resistant insomnia may require combination approaches, alternative medications, or investigation of underlying medical conditions. Sleep specialists can explore advanced interventions including specialized light therapy, chronotherapy, or referral to other medical specialists.
How do I know if my insomnia requires medication or if behavioral approaches are sufficient?
The decision depends on symptom severity, duration, underlying causes, and individual response to initial interventions.
Many sleep specialists in Singapore recommend starting with behavioral approaches like CBT-I, then considering medications if symptoms persist or are severely impacting daily functioning.
Can children and adolescents receive insomnia treatment in Singapore?
Pediatric sleep medicine services are available through public hospitals and specialized private clinics in Singapore.
Treatment approaches for younger patients often emphasize behavioral interventions, sleep hygiene education, and family involvement in treatment planning.

