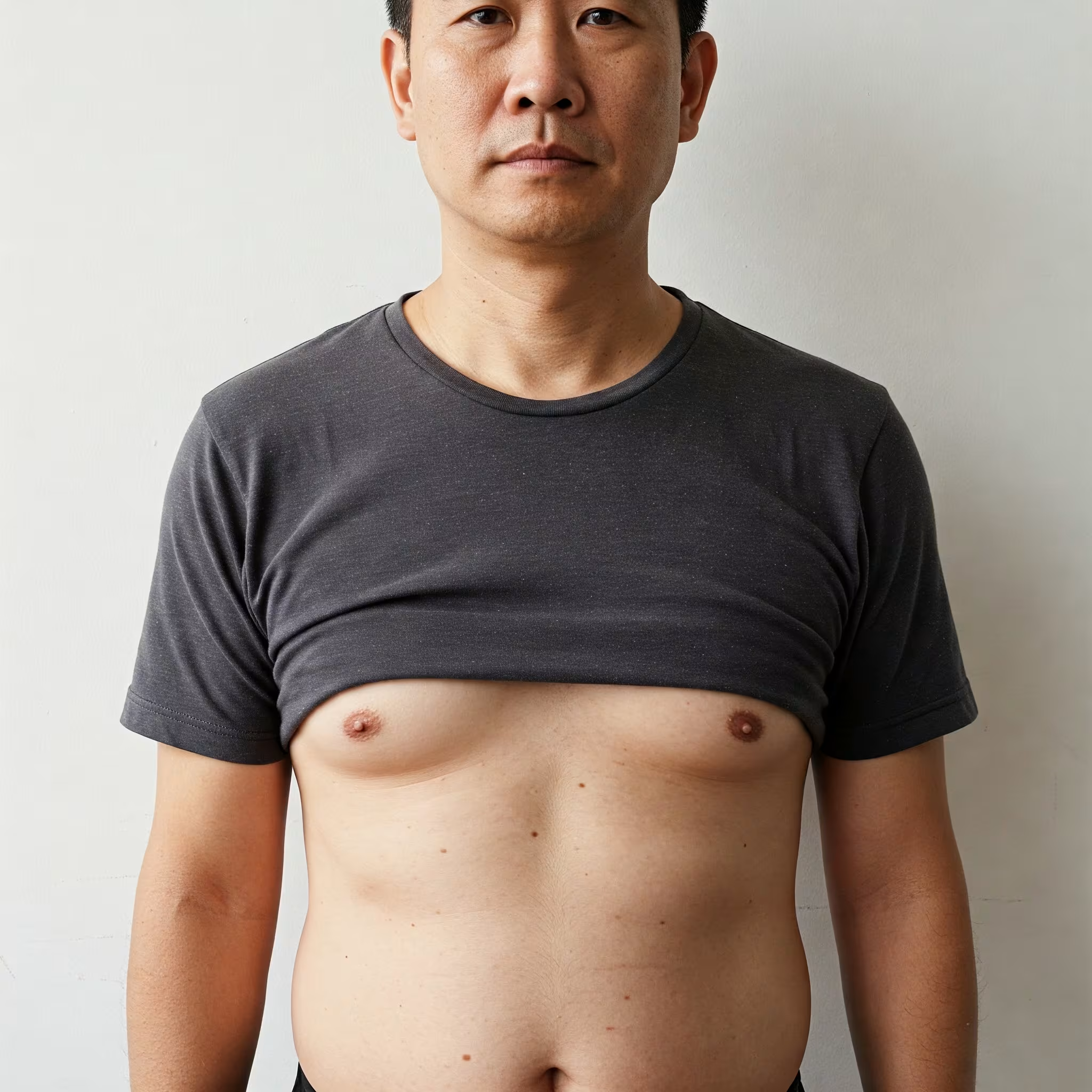
Gynaecomastia, commonly referred to as “man boobs,” is a condition characterized by the enlargement of male breast tissue. This condition affects approximately 24-65% of males ages 50-80, making it much more common than many realize. For those affected, gynaecomastia can cause significant psychological distress, embarrassment, and impact self-esteem.
Many men struggling with this condition find it difficult to seek help due to embarrassment or uncertainty about treatment options. Questions like “Will exercise help?” or “Do I need surgery?” are common among those affected.
This comprehensive guide aims to provide you with everything you need to know about gynaecomastia—from understanding its causes and classifications to exploring the various treatment options available in Singapore, with a focus on surgical interventions for those seeking a permanent solution.
What is Gynaecomastia?
Gynaecomastia is the non-cancerous enlargement of male breast tissue.
This condition develops when there’s an imbalance between the hormones testosterone and estrogen in the male body. While all men produce some estrogen, it’s typically counterbalanced by higher levels of testosterone. When this balance shifts—with either increased estrogen or decreased testosterone—breast tissue can begin to grow.
The condition presents as a firm or rubbery mass that typically starts beneath the nipple and may extend outward over the breast area. It can affect one or both breasts, sometimes asymmetrically, and may be accompanied by tenderness or discomfort.
It’s important to distinguish true gynaecomastia (enlargement of glandular breast tissue) from pseudogynaecomastia, which is caused by fat accumulation in the chest area due to being overweight or obese rather than hormonal changes.
Causes of Gynaecomastia
Gynaecomastia can affect males of all ages, though it most commonly occurs during three main life stages:
Natural Hormonal Changes
- Newborns: Due to estrogen passing from the mother through the placenta
- Puberty: When hormone levels fluctuate significantly (affects 50-60% of adolescent boys)
- Older age: As testosterone production naturally decreases (typically after 50 years)
Medical Conditions
Several medical conditions can disrupt hormone balance and lead to gynaecomastia:
- Liver diseases
- Kidney disease
- Thyroid disorders
- Testicular tumors
- Pituitary disorders
- Klinefelter syndrome
Medications and Substances
Various medications and substances can contribute to breast enlargement in men:
- Heart medications (spironolactone, digoxin, amiodarone)
- Antibiotics and antifungals (ketoconazole, metronidazole)
- Psychiatric medications (haloperidol, diazepam, antidepressants)
- Chemotherapy drugs
- Anabolic steroids
- Recreational drugs including alcohol, amphetamines, and heroin
Lifestyle Factors
- Obesity increases estrogen production and is a common cause of pseudogynaecomastia
- Excessive alcohol consumption
In many cases, particularly persistent adult gynaecomastia, no specific cause can be identified. These cases often respond well to surgical intervention.
Classification of Gynaecomastia
To better understand the severity of the condition and determine appropriate treatment, gynaecomastia is typically classified into four grades:
- Grade 1 (Mild): Enlargement limited to the area of the nipple-areolar complex without excess skin
- Grade 2 (Moderate): Enlargement beyond the nipple-areolar complex without excess skin
- Grade 3 (Moderate): Enlargement beyond the nipple-areolar complex with excess skin
- Grade 4 (Severe): Significant enlargement with excess skin and feminization of the chest
Additionally, gynaecomastia can be classified based on its composition:
- Predominantly glandular tissue
- Predominantly fatty tissue
- Mixed (both glandular and fatty tissues)
Symptoms of Gynaecomastia
The primary symptom of gynaecomastia is the enlargement of breast tissue, which may present as:
- A firm, rubbery disc of tissue beneath the nipple that may extend outward
- Tenderness or sensitivity in the breast area
- Swollen breast tissue
- Nipple sensitivity, especially when rubbing against clothing
- Occasional nipple discharge (rare)
- Pain, particularly in adolescents
Beyond physical symptoms, many men experience significant psychological impact, including:
- Embarrassment and reduced self-confidence
- Avoidance of activities that require removing shirts
- Social anxiety and withdrawal
- Reluctance to engage in intimate relationships
Diagnosis of Gynaecomastia
Proper diagnosis is essential before pursuing treatment for gynaecomastia. The diagnostic process typically involves:
- Medical history: Your doctor will inquire about when you first noticed the breast enlargement, any medications you’re taking, and other relevant health information.
- Physical examination: The doctor will examine your breast tissue to determine if it’s gynaecomastia or pseudogynaecomastia and assess its severity.
- Laboratory tests: Blood tests may be ordered to check hormone levels and rule out underlying medical conditions.
- Imaging: In some cases, a mammogram or ultrasound may be recommended, especially to rule out male breast cancer, which accounts for about 1% of all breast cancers.
Treatment Options for Gynaecomastia
Treatment for gynaecomastia depends on its cause, severity, and the individual’s preferences. Options include:
Non-surgical Approaches
- Observation: For pubertal gynaecomastia, which typically resolves on its own within 2-3 years or by age 21.
- Treating underlying causes: If gynaecomastia is caused by medication or an underlying medical condition, addressing these factors may reverse breast enlargement.
- Weight loss: For pseudogynaecomastia primarily caused by excess fat, diet and exercise can be effective. However, this approach is unlikely to significantly improve true gynaecomastia with prominent glandular tissue.
- Medication: Drugs like tamoxifen and clomiphene, which block estrogen’s effects, may reduce breast size in some cases. These medications are more effective in recent-onset gynaecomastia rather than long-standing cases.
Surgical Approaches
For persistent gynaecomastia, especially cases that have lasted more than a year, surgery is generally the most effective treatment option. Surgical approaches include:
- Liposuction: Removes fatty tissue but cannot effectively address glandular tissue. This is most appropriate for pseudogynaecomastia.
- Excision: Surgical removal of glandular breast tissue through various techniques:
- Mini Excision: A small incision (0.5-1cm) to remove tissue piece by piece
- Open Excision: A larger incision (2-3cm) around the areola for direct visualization and removal
- MELT Technique (Microdebrider Excision and Liposuction Technique): A specialized approach combining liposuction with the use of a microdebrider to remove glandular tissue
- Combined approaches: Many surgeons use a combination of liposuction and excision for optimal results.
- Skin reduction: For grades 3 and 4 with excess skin, additional skin removal procedures may be necessary.
The MELT Technique: An Advanced Surgical Approach
The MELT (Microdebrider Excision and Liposuction Technique) is a hybrid technique developed in Singapore that has gained recognition for treating gynaecomastia effectively with minimal scarring.
How MELT Works:
- A small 5mm incision is made within the nipple’s edge
- Liposuction is performed to remove excess fat tissue
- A microdebrider (a precision cutting tool with suction capability) is used to remove the fibrous glandular tissue layer by layer
- The edges are smoothed, and the incision is closed with absorbable sutures
Benefits of MELT:
- Minimal scarring with incisions hidden within the areola
- Effective removal of both fat and glandular tissue
- Reduced risk of complications including bleeding, scarring, and asymmetry
- Particularly beneficial for thin or muscular individuals with prominent breast discs
- Lower risk of contour irregularities
- Enhanced aesthetic outcomes
Choosing the Right Procedure
The most suitable procedure depends on your specific condition and expectations:
| Procedure | Best For | Anesthesia | Recovery | Scarring | Risk of Residual Tissue |
|---|---|---|---|---|---|
| Liposuction Only | Pseudogynaecomastia (mostly fat) | General | 4 weeks no chest exercise | Minimal | High |
| Excision Only | Small glandular tissue | Local | 6 weeks no chest exercise | Moderate | Low |
| MELT | Mixed tissue or prominent gland | General | 6 weeks no chest exercise | Minimal | Low |
For thin or muscular individuals with little fat and a prominent breast disc, the MELT technique is often considered superior. For those concerned primarily about scarring, MELT or liposuction may be preferred options.
Preparing for Gynaecomastia Surgery
Before undergoing surgery, you’ll need to:
- Consult with a qualified surgeon: Bring all relevant medical reports and discuss your medical history thoroughly.
- Undergo appropriate testing: This may include blood tests, ultrasound, or other imaging to confirm the diagnosis and rule out other conditions.
- Stop certain medications: You’ll need to discontinue blood-thinning medications and supplements that increase bleeding risk.
- Quit smoking: If you smoke, you’ll be asked to stop at least 2 weeks before surgery as smoking impairs healing.
- Discuss expectations: Have a detailed conversation with your surgeon about expected outcomes, recovery, and potential risks.
Cost of Gynaecomastia Surgery in Singapore
In Singapore, the cost of gynaecomastia surgery typically ranges from $6,000 to $13,000. This varies depending on several factors:
- Surgeon’s fee: $3,000-$7,000
- Anesthesia fee: $1,000-$1,500
- Facility fee: $2,000-$4,000
- Medications and consumables: Around $500
Most gynaecomastia surgeries are not covered by Medisave in Singapore.
However, some insurance policies may cover the procedure, especially if it’s symptomatic. It’s advisable to check with your insurance provider or clinic staff for more information.
Recovery and Post-Surgical Care
After gynaecomastia surgery, you can expect:
- Immediate recovery: Most patients are discharged on the same day, with pain managed through oral medications.
- Compression garment: You’ll need to wear a compression vest continuously for 6-12 weeks to reduce swelling, help reshape the chest, and minimize discomfort.
- Activity restrictions:
- Avoid strenuous activity involving the chest and arms for 6 weeks
- Light activities like walking, jogging, and stationary cycling can typically be resumed after 2 weeks
- Follow-up appointments: You’ll have check-ups approximately 5 days post-surgery to remove dressings, and then again after a month.
- Final results: While initial improvements are visible immediately, final results typically take 6 months to fully develop as swelling subsides and tissues settle.
Potential Risks and Complications
While gynaecomastia surgery is generally safe when performed by qualified surgeons, potential complications include:
- Swelling: Expected in the first 1-2 weeks and gradually subsides
- Bleeding or bruising: Risk is minimized by avoiding blood thinners and smoking
- Numbness: Temporary numbness in the chest area is common
- Asymmetry: There may be differences between the two sides
- Under or over-correction: Too much or too little tissue removal can lead to suboptimal results
- Contour irregularities: Uneven chest contour
- Scarring: While usually minimal, some scarring is inevitable
- Nipple complications: Including dimpling, denting, or inversion
- Infection: Rare but possible
Frequently Asked Questions (FAQ)
How common is gynaecomastia?
Gynaecomastia affects 50-65% of males worldwide at some point in their lives, making it the most common male breast disorder.
Will exercise and diet eliminate gynaecomastia?
Exercise and diet can help reduce pseudogynaecomastia (fat-based breast enlargement) but will not effectively reduce true gynaecomastia caused by glandular tissue. For true gynaecomastia with a prominent fibrous disc, surgery is typically the only reliable solution.
At what age should I consider surgery for gynaecomastia?
If you’re a teenager with gynaecomastia, it’s generally recommended to wait until at least 17-18 years of age, as many cases resolve naturally by this time. For persistent cases beyond this age, or for adult-onset gynaecomastia, surgery can be considered at any time.
How painful is gynaecomastia surgery?
Most patients report mild to moderate discomfort rather than severe pain. The discomfort is typically well-managed with oral pain medications for a few days after surgery.
How long will I need to take off work?
Most patients can return to desk jobs within 3-5 days. However, jobs requiring physical exertion, especially those involving chest and arm movements, may require 2-3 weeks off.
Will the breasts grow back after surgery?
Recurrence is uncommon. The removed glandular tissue does not grow back. However, significant weight gain or continued use of medications that cause gynaecomastia could potentially lead to some degree of recurrence.
Is gynaecomastia surgery covered by insurance in Singapore?
In most cases, gynaecomastia surgery is considered cosmetic and not covered by Medisave. However, some private insurance policies may provide coverage, particularly if the gynaecomastia is causing physical symptoms. Check with your insurer for specific coverage details.
How long do I need to wear the compression garment?
Typically, patients are advised to wear the compression garment continuously for 2-3 months after surgery, except when showering.
Will there be visible scars after surgery?
Modern techniques aim to minimize scarring by placing incisions within or around the areola’s edge. These scars generally heal well and become less noticeable over time. The MELT technique, in particular, offers minimal scarring with its small (5mm) incisions.
How do I know if I have true gynaecomastia or pseudogynaecomastia?
True gynaecomastia typically presents as a firm, rubbery disc of tissue directly beneath the nipple. You can check by pinching your chest—if you feel a distinct firm disc that’s different in consistency from surrounding fat, it’s likely true gynaecomastia. Pseudogynaecomastia feels more uniformly soft and fatty.
Can gynaecomastia be a sign of cancer?
While gynaecomastia itself is benign, it’s worth noting that about 1% of all breast cancers occur in men. Signs that warrant immediate medical evaluation include sudden asymmetric enlargement, hard or immobile breast tissue, nipple discharge, skin changes, or lumps in the armpit.
Conclusion
Gynaecomastia affects a significant proportion of the male population and can cause considerable psychological distress. Fortunately, with modern surgical techniques like the MELT procedure, effective treatment is readily available in Singapore with minimal scarring and excellent outcomes.
If you’re considering gynaecomastia surgery, it’s important to consult with a qualified surgeon who can assess your specific condition and recommend the most appropriate treatment approach. With proper diagnosis and treatment, most men achieve significant improvement in both physical appearance and psychological well-being.
Remember that while gynaecomastia can be embarrassing to discuss, it’s a common medical condition that deserves attention and proper treatment. Taking the step to address it can lead to improved self-confidence and quality of life.