What is Vitiligo?
Vitiligo is an acquired skin condition characterized by the progressive loss of skin pigment, resulting in the formation of white patches on the skin.
These patches develop when melanocytes—the cells responsible for producing melanin, which gives our skin its color—are destroyed by the immune system.
This non-contagious condition affects approximately 1 in 100 people worldwide. While vitiligo is relatively common, there remains significant knowledge gaps regarding the condition in Singapore and throughout Asia.
Understanding the Cause of Vitiligo
While the exact underlying cause of vitiligo isn’t fully understood, medical consensus points to an autoimmune response where the body’s immune cells target and destroy melanocytes.
As these pigment-producing cells are destroyed, affected areas gradually lose their color until they appear white.
This depigmentation process can affect one isolated area or multiple regions across the body. The condition can also cause hair growing from affected areas to turn white prematurely.
Symptoms of Vitiligo
Vitiligo is primarily a cosmetic condition that doesn’t cause physical pain or itching. However, its impact can be profound, affecting an individual’s confidence, social interactions, relationships, and even career prospects.
White patches commonly appear in these areas:
- Hands and feet
- Arms and legs
- Face and lips
- Armpits and groin area
- Around the mouth, nose, and eyes
- Inside the mouth and on inner lips
- Abdomen
- Genital and rectal areas
Beyond the visible skin changes, people with vitiligo may experience:
- Increased sensitivity to sunlight and higher risk of sunburn in affected areas
- Premature whitening of hair in affected regions (including eyebrows and eyelashes)
- In rare cases, eye problems related to pigmentation changes
Types of Vitiligo
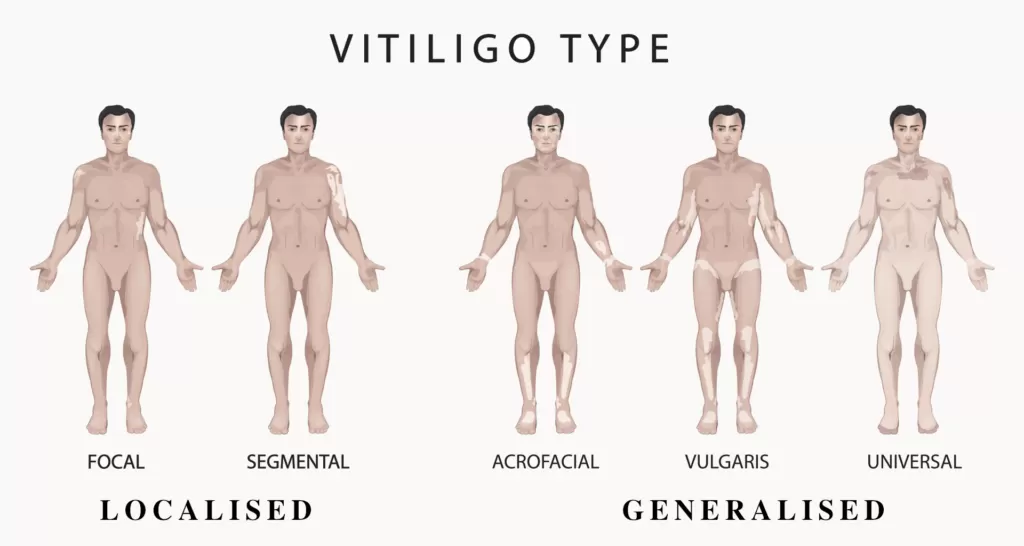
There are several distinct types of vitiligo:
- Generalized vitiligo: The most common form, characterized by symmetrical, widespread white patches that can affect any part of the body.
- Segmental vitiligo: Affects only one side or part of the body, usually appearing in a specific segment or area, and often begins at a younger age.
- Focal vitiligo: Features a few scattered white patches in one area and is generally less widespread than other types.
- Mucosal vitiligo: Affects mucous membranes like the inside of the mouth or nose and is often associated with generalized vitiligo.
Famous Personalities with Vitiligo
Several notable personalities have vitiligo, helping to increase awareness and acceptance of the condition:
- Michael Jackson: Perhaps the most famous person who lived with vitiligo. After his death, medications used to treat vitiligo (hydroquinone and benoquin) were found in his home. These prescription topical medicines are used to lighten parts of skin not already affected by vitiligo to create a more uniform appearance. June 25, the anniversary of Jackson’s death, is now recognized as World Vitiligo Day.
- Winnie Harlow: Known from America’s Next Top Model, she has become an advocate for vitiligo awareness and acceptance. Despite being bullied in school, she has built a successful modeling career and received recognition as one of BBC’s 100 Women in 2016. She has spoken out against being labeled as a “vitiligo sufferer,” emphasizing that while she has vitiligo, it doesn’t define her.
- Other celebrities with vitiligo include Joe Rogan and Amitabh Bachchan.
Common Misconceptions About Vitiligo
There are many myths surrounding vitiligo that contribute to stigmatization. Here are facts to counter these misconceptions:
Myth: Vitiligo is infectious.
- Fact: Vitiligo is not contagious. You can have normal physical contact with people who have vitiligo without any risk of contracting the condition.
Myth: Vitiligo is caused by having parents of different races or mixed heritage.
- Fact: Vitiligo has no connection to ethnicity or racial background. People with vitiligo often have normal skin pigmentation during childhood before developing the condition.
Myth: Only people with darker skin develop vitiligo.
- Fact: Vitiligo affects people of all skin tones, though it may be more visually apparent on darker skin.
Myth: Certain foods like dairy products can worsen vitiligo.
- Fact: There is no strong scientific evidence linking specific foods to vitiligo progression, though a balanced diet supports overall immune health.
Myth: People with vitiligo have reduced intelligence.
- Fact: Vitiligo has absolutely no impact on cognitive abilities or academic performance.
Myth: Vitiligo is the same as albinism, leprosy, or skin cancer.
- Fact: While these conditions may share certain visual similarities, they have different causes, progressions, and treatments.
Myth: Sun exposure causes vitiligo.
- Fact: While sun exposure can make vitiligo more noticeable and may trigger flare-ups, it’s not a direct cause of the condition.
Risk Factors and Triggers for Vitiligo
Vitiligo can affect anyone regardless of age, gender, or ethnicity, though it’s most commonly diagnosed between ages 10-30. Several factors may increase susceptibility:
- Autoimmune conditions: People with thyroid disorders, type 1 diabetes, or other autoimmune conditions have higher risk.
- Family history: Those with relatives who have vitiligo may have a genetic predisposition.
- Physical trauma: Skin injuries like cuts, burns, or bruises can trigger vitiligo development in predisposed individuals (Koebner phenomenon).
- Stress: Some patients report flare-ups during periods of intense physical or emotional stress.
- Chemical exposure: Contact with certain industrial chemicals containing phenols may trigger vitiligo in some cases.
Is Vitiligo Hereditary?
There appears to be a genetic component to vitiligo, as it sometimes runs in families. However, genetics alone doesn’t determine whether someone will develop the condition. Environmental factors, triggers, and other conditions must often be present.
Interestingly, even identical twins (with identical genetic makeup) have only about a 23% chance of both developing vitiligo in their lifetime. Rather than considering vitiligo strictly hereditary, it’s more accurate to say that the tendency to develop vitiligo can be inherited.
Can Vitiligo Go Away on Its Own?
In some cases, vitiligo patches may disappear without treatment as melanocytes multiply and repopulate affected areas. However, this natural repigmentation is typically very slow and uncommon, particularly if:
- The condition hasn’t stabilized (new patches are still forming)
- The affected areas are extensive
Most patients experience minimal natural repigmentation even after many years. For those seeking faster results, medical treatments are available.
Diagnosis of Vitiligo
Diagnosing vitiligo typically involves:
- Clinical examination: A thorough examination of the entire skin surface often reveals additional areas of pigment loss that patients may not have noticed, such as on the back, scalp, or genital areas.
- Wood’s lamp examination: This specialized UV light causes depigmented areas to fluoresce white, helping doctors identify areas of partial pigment loss not visible under normal lighting.
- Medical history: Doctors will ask about recent infections, injuries, stress, allergies, or changes in skin exposure, including new soaps or detergents.
- Differential diagnosis: Doctors need to rule out similar-looking conditions such as:
- Postinflammatory hypopigmentation
- Chemically induced depigmentation
- Pityriasis alba
- Tinea versicolor
- Idiopathic guttate hypomelanosis
- Additional testing: In some cases, blood tests may be ordered to check for associated autoimmune conditions.
Treatment Options for Vitiligo in Singapore
There is no one-size-fits-all treatment for vitiligo. Early diagnosis and treatment generally lead to better outcomes by limiting depigmentation and mitigating psychological effects.
Treatment success depends heavily on consistency, compliance, and persistence with the prescribed regimen.
Topical Treatments
- Topical Corticosteroids
- Often the first-line treatment for limited vitiligo (affecting less than 10% of body)
- Works by suppressing the inflammatory response
- Side effects with prolonged use include skin thinning, easy bruising, visible blood vessels, and potential systemic effects
- Topical Calcineurin Inhibitors (e.g., tacrolimus/Protopic)
- Non-steroidal alternatives, particularly useful for sensitive areas like around the eyes
- Avoids steroid-associated side effects
- May cause temporary burning sensation that typically resolves with continued use
- Topical Vitamin D (e.g., calcipotriol, tacalcitol)
- Inhibits immune cell activity and promotes melanocyte growth
- Often used in combination with phototherapy
- Also used for other conditions like psoriasis
Phototherapy
Phototherapy involves exposing affected skin to ultraviolet light to stimulate melanocyte proliferation. Current approaches include:
- Narrowband UVB Phototherapy
- The most commonly used form for vitiligo
- Uses a specific wavelength of UVB light for better repigmentation rates
- Generally well-tolerated, even by children and pregnant women
- Requires 2-3 sessions weekly, with visible results typically appearing after 10-30 sessions
- Full repigmentation may take longer
- Main concerns include sunburn and possible reactivation of herpes simplex
- Excimer Light/Laser
- Targeted phototherapy for small, localized areas
- Particularly effective for facial vitiligo
- Treatment administered 2-3 times weekly
Systemic Treatments
- Oral Corticosteroids
- Used for rapidly progressing vitiligo affecting large body areas
- Helps stabilize the condition
- Significant side effect profile requires careful monitoring
- JAK Inhibitors
- Newer treatment option showing promise
- Works by blocking specific immune pathways
Surgical Options
Surgical approaches are generally reserved for stable vitiligo (no new or enlarging patches for 6-12 months) that hasn’t responded to other treatments:
- Tissue Grafting
- Includes epidermal grafts, suction blister grafts, and mini-punch grafting
- Involves transplanting healthy skin tissue to affected areas
- Melanocyte Transfer
- More sophisticated approach involving grafting the patient’s own melanocytes onto vitiligo areas
- Studies show up to 90% of patients with segmental vitiligo achieve good to complete recovery
- Can be performed on an outpatient basis and is approved by Singapore’s Ministry of Health
Other Management Approaches
- Camouflage Cosmetics
- Provide good color-matching and coverage, particularly useful for facial vitiligo
- Sunscreen
- Essential as depigmented areas are highly susceptible to sunburn
- Broad-spectrum, high SPF protection recommended
Treatment Efficacy: What the Research Shows
Recent Singapore-based research on vitiligo treatment has yielded promising results:
- Cellular grafting achieved 65% or higher repigmentation within six months for patients with stable vitiligo, with results maintained after one year.
- 83% of patients who underwent noncultured cellular grafting achieved good to excellent repigmentation at the five-year mark.
- Phototherapy has proven effective and safe for treating vitiligo in Asian children, including those with darker skin tones. Patients with generalized vitiligo responded better to phototherapy than those with segmental vitiligo.
- Proper health consultation has been shown to help patients maintain psychological health and alleviate symptoms of depression.
Treatment Cost in Singapore
Vitiligo treatment costs in Singapore vary based on several factors. Here’s an approximate guide:
| Treatment/Medication | Approximate Cost (SGD) | Frequency | Notes |
|---|---|---|---|
| Topical corticosteroids | $100+ | Applied twice daily | Cost varies with affected area size |
| Topical calcineurin inhibitors | $100+ | As prescribed | |
| Oral corticosteroids | $30-40 | Often 2 days weekly for 12 weeks | |
| Phototherapy | $50+ per session | 2-3 times weekly | 10-30+ sessions typically needed |
| Excimer Treatment | $100+ per session | As prescribed | More suitable for facial areas |
| Surgical procedures | Varies widely | One-time procedure | Only for stable vitiligo (6-12 months) |
Subsidies for Vitiligo Treatment
In Singapore, certain vitiligo treatments are eligible for financial assistance:
- For patients over 60, treatments and medications at polyclinics, specialist outpatient clinics, and CHAS general practitioner clinics are claimable under Flexi-Medisave.
- Vitiligo is not classified as a Chronic Disease Management Programme condition, so MediSave500 claims aren’t applicable.
- Inpatient treatments like skin grafting surgery follow standard inpatient medical treatment claim guidelines.
When to Seek Treatment
If you suspect you or someone you know has vitiligo, consult a doctor promptly. Early management can help slow progression and improve outcomes. However, those with long-standing vitiligo can still benefit from treatment, though individual response may differ.
Some people choose not to seek treatment, instead embracing their unique appearance. This is a personal decision, though many with customer-facing jobs or careers may opt for treatment to minimize potential professional impact.
Choosing a Vitiligo Specialist in Singapore
When selecting a doctor for vitiligo treatment, consider:
- Approach and bedside manner: Find a doctor whose perspective aligns with yours and who understands both the physical and psychological aspects of vitiligo.
- Clinic location: Since treatment often requires multiple regular visits, accessibility is important.
- Medical team: Experienced nursing staff contribute significantly to treatment effectiveness.
- Facilities: If considering phototherapy, understand the specific devices used, as some are more effective than others.
- Experience: A doctor who has treated numerous vitiligo cases will have broader knowledge of treatment options and potential outcomes.
Look for a holistic approach that addresses not just skin concerns but overall well-being.
Questions to Ask During Your First Consultation
Prepare to discuss:
- When you first noticed the white patches
- Whether you’ve observed growth or changes in response to certain life events
- Any previous treatments (conventional or alternative)
- Family history of vitiligo or autoimmune conditions
- Occupational exposures and stressors
- Medical history, particularly autoimmune conditions
Bringing photos documenting the progression of affected areas can be helpful.
Preventing Vitiligo Progression
While vitiligo itself cannot be prevented, identifying and avoiding personal triggers may help reduce flare-ups:
- Use sun protection to prevent sunburn
- Minimize physical trauma to the skin when possible
- Develop healthy stress management techniques
- Maintain a balanced, nutritious diet rich in various colored fruits and vegetables to ensure adequate micronutrient intake
Living with Vitiligo
Living well with vitiligo extends beyond medical treatment. Remember that vitiligo is just one aspect of your overall health:
- Maintain an active social life
- Set meaningful personal and professional goals
- Consider connecting with support groups
- Focus on overall physical and mental wellness
- Surround yourself with supportive people who value you for who you are, not how you look
Frequently Asked Questions
Is vitiligo contagious?
No, vitiligo is not contagious. You cannot “catch” vitiligo through physical contact, sharing food, or any other form of interaction with someone who has the condition.
Does vitiligo affect overall health?
Vitiligo itself doesn’t affect physical health beyond increased sun sensitivity in affected areas. However, people with vitiligo have a higher likelihood of developing certain autoimmune conditions, so regular health monitoring is recommended.
Can children develop vitiligo?
Yes, vitiligo can develop at any age, though it most commonly appears between ages 10-30.
Is vitiligo more common in certain ethnic groups?
Vitiligo affects people of all ethnicities equally, though it may be more visually apparent on darker skin tones.
Can diet affect vitiligo?
There’s no strong scientific evidence linking specific foods to vitiligo progression or improvement. However, a balanced diet supports overall immune function and general health.
Is vitiligo progressive?
Vitiligo can be progressive, with new patches appearing over time. The rate of progression varies significantly between individuals—some experience rapid spreading, while others have stable patches for years.
Can stress cause vitiligo?
Stress itself doesn’t cause vitiligo, but it may trigger flare-ups in people predisposed to the condition.
Does vitiligo require lifelong treatment?
While there’s no permanent cure, treatment can effectively manage vitiligo. Some people achieve complete repigmentation with appropriate treatment, though maintenance therapy may be needed to prevent recurrence.
Can I use regular makeup to cover vitiligo patches?
Regular makeup can provide some coverage, but specialized camouflage cosmetics designed for skin conditions typically offer better color-matching and durability.
Are there any new treatments on the horizon?
Research into vitiligo treatments continues to evolve. JAK inhibitors represent one of the newest treatment approaches showing promise, and ongoing research into the immunological basis of vitiligo may lead to additional targeted therapies in the future.

