In Singapore, approximately 15% of the population experiences symptoms of acid reflux, making it a prevalent digestive concern among locals.
What might seem like occasional discomfort after a heavy meal can potentially develop into a chronic condition that significantly impacts quality of life.
Acid reflux, gastric reflux, and Gastroesophageal Reflux Disease (GERD) are terms often used interchangeably, but they represent different stages of the same digestive issue.
Understanding the differences between these conditions, their causes, symptoms, and available treatment options is crucial for proper management and prevention of complications.
What is Acid Reflux?
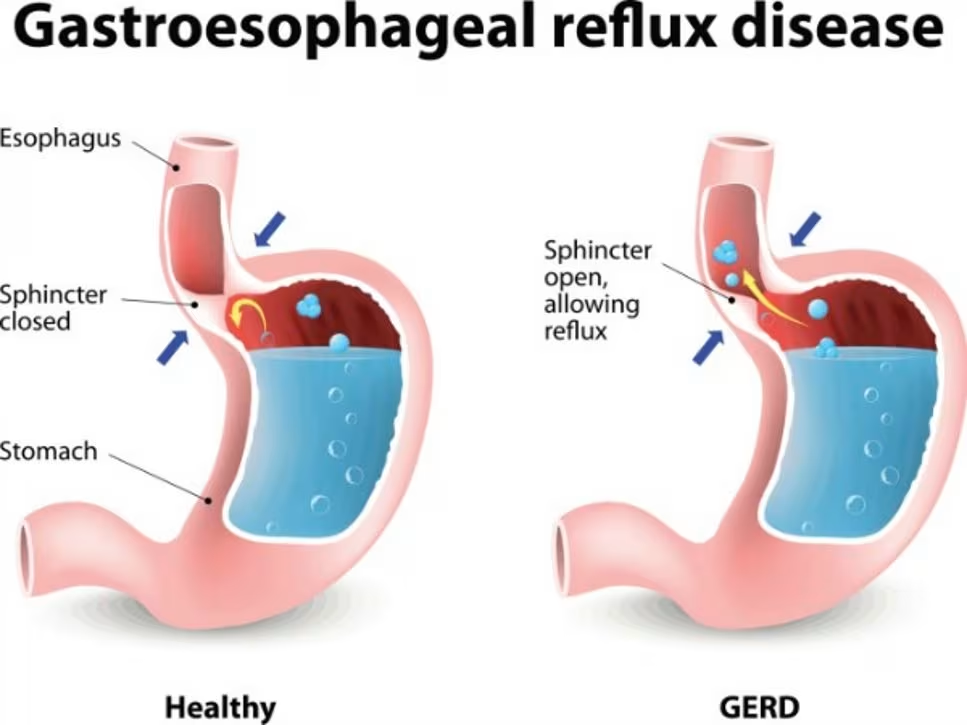
Acid reflux occurs when acidic contents from the stomach flow back into the oesophagus, the muscular tube connecting your mouth to your stomach.
This backflow happens when the Lower Oesophageal Sphincter (LOS) relaxes abnormally or weakens. The LOS is a ring of muscle that normally acts as a valve, regulating the flow of food from the oesophagus into the stomach while preventing stomach acid from flowing back up.
When stomach acid travels up into the oesophagus, it can cause irritation and inflammation of the oesophageal lining, leading to various uncomfortable symptoms.
Occasional acid reflux is common and usually not a cause for concern, but frequent episodes may indicate a more serious condition.
Related article: Irritable Bowel Syndrome (IBS): Causes, Symptoms and Treatment in Singapore
Acid Reflux vs. GERD: Understanding the Distinction
While acid reflux refers to the occasional backflow of stomach acid into the oesophagus, GERD represents a chronic and more severe form of this condition. Here’s how to distinguish between them:
Acid Reflux
- Occurs occasionally, typically after large meals or lying down after eating
- Symptoms may include heartburn and regurgitation
- Can usually be managed with lifestyle changes and over-the-counter medications
GERD
- Chronic condition where acid reflux occurs more than twice a week
- Symptoms are persistent and more intense
- Can lead to tissue damage and scar tissue formation
- May require prescription medications or surgical intervention
- Carries risk of long-term complications if left untreated
You might be interested: Functional Dyspepsia Treatment in Singapore
Heartburn

It’s important to note that heartburn is a symptom, not a condition in itself. The term “heartburn” can be misleading as it suggests a connection to the heart, but this symptom actually originates from the oesophagus.
It’s characterized by a burning sensation behind the breastbone that often radiates upward toward the throat.
Stages of GERD
GERD can be classified into four stages based on the severity of acid reflux:
Stage 1: Mild GERD
- Acid reflux occurs once or twice a month
- May experience heartburn (burning pain behind the breastbone)
- Pain is usually tolerable
- Can be managed with over-the-counter medications and lifestyle changes
Stage 2: Moderate GERD
- Acid reflux and heartburn occur more frequently with increasing intensity
- Pain may affect daily activities
- May require daily prescription acid reflux medication
- Over-the-counter medications may become ineffective
Stage 3: Severe GERD
- Symptoms are painful and persistent despite medication
- May include heartburn, chest pain, difficulty swallowing, regurgitation of food or stomach acid
- Persistent dry cough and frequent feeling of a lump in the throat
- Quality of life is severely affected
- May require surgical intervention
Stage 4: Precancerous Lesions or Cancer
- Repeated damage from years of severe untreated acid reflux may lead to Barrett’s oesophagus, a precancerous condition
- If left untreated, may progress to oesophageal adenocarcinoma, a rare cancer
Related article: Celiac Disease Treatment in Singapore
Common Symptoms of Acid Reflux and GERD
The symptoms of acid reflux and GERD can vary widely in presentation and intensity, with GERD symptoms typically being more frequent and severe. Common symptoms include:
Typical Symptoms:
- Heartburn: A burning sensation in the chest, particularly after meals or when lying down
- Regurgitation: The sensation of acid or food backing up into the throat or mouth, often leaving a sour or bitter taste
- Dysphagia: Difficulty swallowing or feeling that food is stuck in the throat
- Chest Pain: Discomfort or pain in the chest that can sometimes mimic heart problems
Atypical Symptoms:
- Chronic Cough: A persistent cough, especially at night
- Sore Throat: Chronic irritation leading to soreness or a scratchy feeling
- Hoarseness: Changes in voice quality due to irritation of the vocal cords
- Bad Breath: Persistent bad breath resistant to oral hygiene
- Difficulty Breathing: Respiratory symptoms, especially at night
- Unexpected Weight Loss: In severe cases
Common Causes and Risk Factors of GERD in Singapore
Several factors can contribute to the development of GERD. Understanding these risk factors is essential for prevention and management.
Physical Conditions:
- Obesity: Carrying extra weight increases intra-abdominal pressure, reduces LOS pressure, and impairs gastric emptying
- Pregnancy: Hormonal changes during pregnancy can decrease LOS pressure and affect digestive tract muscles
- Hiatal Hernia: When the top portion of the stomach protrudes through the diaphragm into the chest
- Connective Tissue Disorders: These can affect oesophageal function as the LOS consists of connective tissues
- Scleroderma: An autoimmune disease resulting in ineffective peristalsis of the oesophagus
- Gastroparesis: Impaired ability of the stomach to empty properly
Lifestyle Factors:
- Smoking: Weakens the LOS and impairs saliva production, which helps neutralize stomach acid
- Dietary Choices: Consuming large meals or eating late at night
- Specific Foods and Beverages: Regular consumption of fatty, spicy, or fried foods; chocolate; mint; garlic; onion
- Beverages: Frequent intake of carbonated drinks, alcohol, or coffee
- Medications: Certain medications such as calcium channel blockers, antihistamines, painkillers, sedatives, and some asthma medications
How is GERD Diagnosed?
Accurate diagnosis is crucial for effective treatment of GERD. While a physician may initially diagnose based on symptoms, several diagnostic tests may be recommended to confirm the diagnosis and assess the severity of the condition.
Gastroscopy (Upper Endoscopy)
A gastroscopy, also known as an Oesophago-Gastro-Duodenoscopy (OGD), allows the gastroenterologist to examine the upper gastrointestinal tract for structural abnormalities. This procedure involves inserting a flexible endoscope through the mouth to visualize the oesophagus, stomach, and upper small intestine.
A gastroscopy can also be used to collect a small tissue sample (biopsy) from the oesophagus to test for conditions such as Barrett’s oesophagus or oesophageal cancer.
Ambulatory (24-hour) Oesophageal pH Test
This test measures the amount of acid that flows into the oesophagus over a 24-hour period. It involves:
- Insertion of a catheter with a pH probe through the nose, positioned five centimeters above the LOS
- Recording of acid reflux episodes in relation to meals and daily activities
- Alternative wireless capsule option for patients who find the catheter uncomfortable
Oesophageal Manometry
This test evaluates the muscle function of the oesophagus and the LOS:
- A catheter is inserted through the nose into the oesophagus after applying numbing medication
- The patient swallows small sips of water while a computer measures the speed, pattern, and strength of oesophageal muscle contractions
- Particularly useful before surgery to ensure that the oesophageal muscles are functioning well
Barium Contrast Radiography
This X-ray study involves ingesting barium pills or solution that coats the oesophagus and digestive tract, making it easier for the gastroenterologist to visualize the silhouette of the tract and detect any abnormalities.
What is Barrett’s Oesophagus?
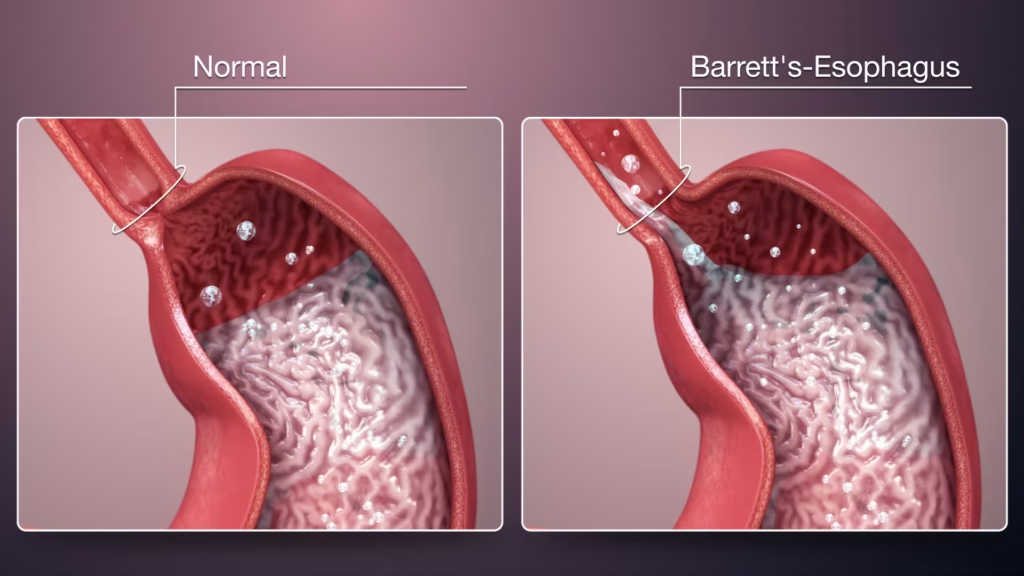
Barrett’s oesophagus is a serious complication of long-standing GERD, where the oesophageal tissue becomes damaged (thickens and reddens) due to chronic exposure to stomach acid. In this condition, the cells lining the oesophagus change into cells resembling those found in the intestines, a process called intestinal metaplasia.
This transformation increases the risk of developing oesophageal adenocarcinoma, a type of cancer. While many patients with Barrett’s oesophagus may not experience symptoms different from regular GERD, some may develop:
- Painful swallowing
- Chronic sore throat
- Sour taste in the mouth
- Bad breath
- Unexpected weight loss
- Bloody stools
- Vomiting
Regular monitoring through endoscopy is recommended for patients diagnosed with Barrett’s oesophagus to watch for early signs of cancer development.
Treatment Options for GERD in Singapore
Treatment for GERD typically follows a step-up approach, starting with lifestyle modifications before progressing to medications and, in some cases, surgical interventions.
Lifestyle Changes
For individuals with mild GERD, lifestyle modifications can be highly effective:
Dietary Adjustments:
- Eat smaller, more frequent meals
- Avoid eating 2-3 hours before bedtime
- Sit upright for a few hours after meals
- Maintain a healthy weight
- Reduce pressure on the stomach
- Stay hydrated
Foods to Avoid:
- Fatty and oily foods and beverages
- Spicy foods
- Citrus fruits
- Carbonated drinks
- Tomato and tomato-based foods
- Fried foods
- Onion and garlic
- Mint
- Chocolate
- Coffee
Additional Measures:
- Quit smoking
- Elevate the head of the bed if experiencing nighttime symptoms
- Avoid tight-fitting clothing that increases abdominal pressure
Medications
When lifestyle and dietary changes are insufficient, medications may be prescribed:
Antacids
These over-the-counter medications neutralize stomach acid, making the stomach contents less corrosive and providing short-term relief for acid reflux.
Histamine 2 Receptor Antagonists (H2RAs)
H2RAs decrease stomach acid production by reversibly binding to histamine receptors and blocking the production of histamine on gastric parietal cells in the stomach. Examples include famotidine and cimetidine.
Proton Pump Inhibitors (PPIs)
PPIs block and reduce stomach acid production, reducing the severity and frequency of acid reflux and allowing time for oesophageal tissue to heal. Common PPIs include omeprazole, esomeprazole, pantoprazole, rabeprazole, and dexlansoprazole.
Potassium Competitive Acid Blockers (PCABs)
Newer medications such as vonoprazan work by competitively inhibiting the potassium-binding site of gastric hydrogen/potassium ATPase.
Surgical and Endoscopic Procedures
For patients who do not respond to medication or have severe complications, surgical interventions may be considered:
Laparoscopic Surgery
Minimally invasive procedures performed through small incisions:
- Nissen Fundoplication: Part of the upper stomach is wrapped around the LOS, tightening the sphincter and preventing acid reflux
- Anterior Partial Fundoplication: Similar to Nissen fundoplication but with the upper stomach wrapping only partially around the oesophagus
- Magnetic Sphincter Augmentation (MSA): Implantation of a small device made of tiny magnetic titanium beads (LINX) to strengthen the sphincter
- Bariatric Surgery: For obese patients to reduce meal size and stomach pressure
Endoscopic Surgery (Endoluminal Therapy)
Procedures performed using tools attached to an endoscope inserted through the mouth:
- Transoral Incisionless Fundoplication (TIF): Creates folds at the distal oesophagus using a device attached to the endoscope, strengthening the barrier against acid reflux
- Endoscopic Radiofrequency (RF) Ablation: Uses low-energy radiofrequency pulses to strengthen the sphincter without damaging surrounding tissue
Complications of Untreated GERD
If left untreated, GERD can lead to several complications:
- Oesophagitis: Inflammation of the oesophageal lining, which may result in bleeding, ulcers, and painful swallowing
- Oesophageal Strictures: Narrowing of the oesophagus due to scar tissue formation, causing difficulty swallowing
- Barrett’s Oesophagus: Changes in the oesophageal lining that increase the risk of cancer
- Respiratory Issues: Including chronic cough, asthma, or pneumonia due to aspiration of acid into the lungs
- Sleep Disturbances: Nighttime reflux can significantly disrupt sleep patterns
When to Seek Medical Attention
It’s important to consult a gastroenterologist if you:
- Experience persistent GERD symptoms despite over-the-counter medications and lifestyle changes
- Have difficulty swallowing or feel food getting stuck
- Experience unexplained weight loss
- Have recurrent vomiting episodes
- Notice black or tarry stools (indicates bleeding)
- Experience chest pain, especially when accompanied by shortness of breath (note that chest pain can sometimes indicate heart issues rather than GERD)
Prevention of GERD
Preventing GERD involves many of the same strategies used to manage the condition:
- Maintain a healthy weight
- Avoid trigger foods and beverages
- Eat smaller meals
- Allow 2-3 hours between eating and lying down
- Quit smoking
- Limit alcohol consumption
- Avoid tight-fitting clothing around the waist
- Manage stress effectively
- Take medications as prescribed
Can GERD be Cured?
In some cases, GERD symptoms may resolve completely, particularly when associated with temporary conditions like pregnancy. In cases where obesity is the underlying cause, weight management can lead to significant improvement or resolution of symptoms.
For most patients, however, GERD is a chronic condition that requires ongoing management. With proper treatment—combining lifestyle modifications, medications, and in some cases, surgical interventions—most people can effectively control their symptoms and prevent complications.
Surgery is typically only recommended when patients do not respond to medication or when complications such as cancer have occurred. Otherwise, medication along with lifestyle management can keep symptoms under control.
GERD in Singapore: The Local Context
In Singapore, the prevalence of GERD has been increasing, with approximately 15% of the population experiencing symptoms. This trend is likely influenced by:
- Increasingly sedentary lifestyles
- Rising obesity rates
- Stress from the fast-paced urban environment
- Dietary habits including the consumption of spicy local cuisines and late-night eating culture
Local gastroenterologists report that many Singaporeans delay seeking treatment for GERD symptoms, often self-medicating with over-the-counter antacids until symptoms become severe. Raising awareness about the potential complications of untreated GERD is therefore an important public health concern in Singapore.
Frequently Asked Questions (FAQ)
What is the difference between acid reflux, heartburn, and GERD?
Acid reflux is the backflow of stomach acid into the oesophagus. Heartburn is a symptom of acid reflux, characterized by a burning sensation in the chest. GERD is a chronic, more severe form of acid reflux that occurs more than twice a week and can lead to complications if left untreated.
Can GERD go away on its own?
Occasional acid reflux may resolve on its own, but GERD is typically a chronic condition that requires management. In some cases, such as pregnancy-related GERD, symptoms may resolve after giving birth. For obesity-related GERD, weight loss can significantly improve or resolve symptoms.
What foods should I avoid if I have GERD?
Common trigger foods include spicy, fatty, or fried foods; chocolate; mint; garlic; onion; tomato-based foods; citrus fruits; carbonated beverages; coffee; and alcohol. However, triggers can vary from person to person, so keeping a food diary can help identify your specific triggers.
Is GERD dangerous?
While GERD itself is not life-threatening, untreated chronic GERD can lead to serious complications, including oesophagitis, strictures, Barrett’s oesophagus (which increases the risk of oesophageal cancer), and respiratory problems due to aspiration of stomach acid.
How is GERD different from ordinary indigestion?
Indigestion (dyspepsia) is discomfort centered in the upper abdomen and may include feelings of fullness, bloating, or nausea after eating. GERD specifically involves the backflow of stomach acid into the oesophagus, with symptoms like heartburn and regurgitation. While they can occur together, they are distinct conditions.
Can stress cause GERD?
Stress doesn’t directly cause GERD, but it can exacerbate symptoms by increasing stomach acid production, slowing digestion, and triggering behaviors that worsen GERD, such as consuming comfort foods, smoking, or drinking alcohol.
How long does it take for GERD medication to work?
Antacids provide almost immediate relief but are short-acting. H2 blockers typically start working within an hour and last for several hours. PPIs may take 1-4 days to reach maximum effectiveness and are designed for longer-term acid reduction.
Can children get GERD?
Yes, children of all ages can develop GERD. In infants, it often presents as frequent spitting up, irritability during feeding, and poor weight gain. In older children, symptoms mirror those in adults. Many children outgrow GERD as their digestive systems mature.
Is surgery for GERD a last resort?
Surgery is typically considered when:
- Symptoms persist despite optimal medical therapy
- Patients cannot tolerate medications
- Complications like severe oesophagitis, strictures, or Barrett’s oesophagus develop
- There is a large hiatal hernia
- Patients prefer a long-term solution over lifetime medication
How does obesity contribute to GERD?
Excess weight increases pressure on the abdomen, which can push stomach contents upward and impair the function of the LOS. Obesity also affects hormones that regulate digestion and can slow gastric emptying, increasing the risk of reflux.
Can GERD cause bad breath?
Yes, GERD can cause bad breath (halitosis). When stomach acid flows back into the oesophagus and throat, it can create an environment where bacteria thrive, leading to unpleasant breath odor.
Is GERD genetic?
There appears to be a genetic component to GERD. Studies show that the condition can run in families, suggesting that inherited factors may influence susceptibility to GERD, possibly through effects on sphincter function, tissue resistance, or stomach acid production.
How is GERD diagnosed in pregnant women?
GERD is common during pregnancy and is typically diagnosed based on symptoms. Invasive diagnostic tests are usually avoided unless complications are suspected. Treatment focuses on lifestyle modifications and safe medications like antacids.
Can GERD symptoms mimic heart attack?
Yes, chest pain from GERD can mimic heart attack symptoms, sometimes making it difficult to distinguish between the two. If you experience severe chest pain, especially if accompanied by shortness of breath, arm or jaw pain, or sweating, seek emergency medical attention to rule out a heart attack.
Conclusion
Gastroesophageal reflux disease is a common digestive condition affecting many Singaporeans. While it can significantly impact quality of life, most cases can be effectively managed through a combination of lifestyle modifications, dietary changes, and appropriate medications.
Understanding the difference between occasional acid reflux and chronic GERD is crucial for proper management and prevention of complications. If you experience persistent or worsening reflux symptoms, consulting a gastroenterologist is recommended for proper diagnosis and personalized treatment.
With proper management, most individuals with GERD can lead normal, symptom-free lives while minimizing the risk of long-term complications.

