Understanding Irritable Bowel Syndrome
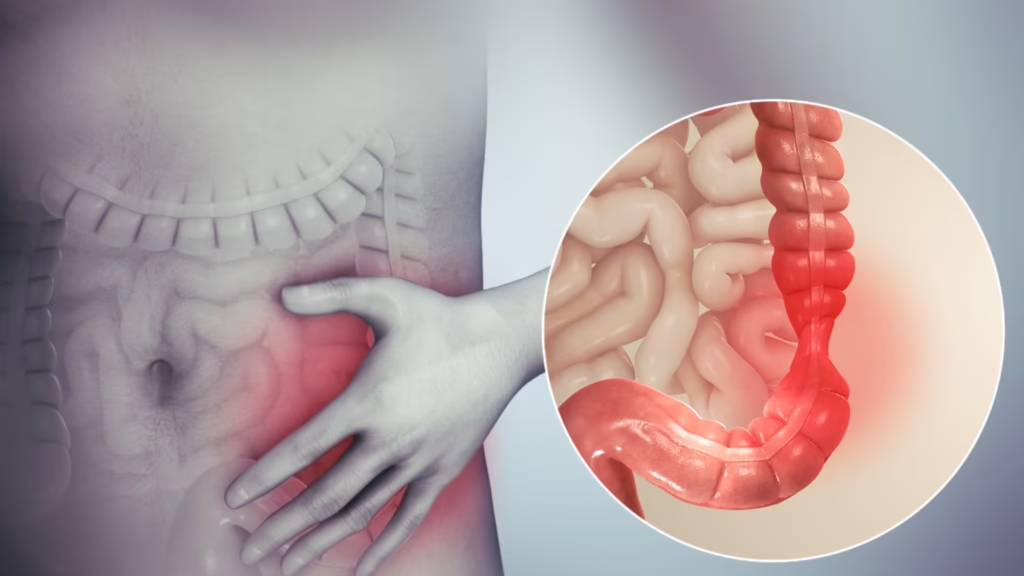
Irritable Bowel Syndrome (IBS) is a prevalent chronic gastrointestinal disorder characterized by a combination of persistent and recurrent abdominal pain along with abnormal bowel habits.
Often referred to as “sensitive gut,” “spastic colon,” or “nervous colon,” IBS affects approximately 10% of Singapore’s population, compared to about 20% in the United States.
The condition tends to affect more women than men and typically occurs most frequently in adults in their 30s and 40s.
IBS is a functional disorder, meaning that while symptoms are real and can significantly impact quality of life, they are not associated with structural problems like ulcers or cancers.
This often results in normal findings in blood tests, endoscopies, or scans for patients with IBS.
Related article: Acid Reflux and GERD in Singapore: Causes, Symptoms, and Treatments
Common Causes and Mechanisms of IBS
Although the exact cause of IBS remains unknown, medical understanding has progressed beyond viewing it as merely a psychological problem. Several mechanisms contribute to IBS symptoms:
- Altered Bowel Motility: The gut may move faster or slower than normal, or experience spasms, leading to diarrhea or constipation.
- Visceral Hypersensitivity: People with IBS tend to be more aware of their gut contractions and movements, experiencing pain during normal activities like eating or bowel movements.
- Brain-Gut Axis Dysregulation: Communication between the brain and gut is disrupted, potentially leading to an inability to regulate pain or excessive signals causing diarrhea.
- Dysbiosis: An imbalance where beneficial bacteria are replaced by harmful bacteria, resulting in increased sensitivity of intestinal nerves or excessive fermentation of food.
- Post-Infectious IBS: Approximately 30% of patients report IBS symptoms after recovering from gastroenteritis.
- Psychological Factors: Stress often triggers IBS symptoms, and managing chronic IBS symptoms can itself become stressful, creating a cycle.
- Neurotransmitter Imbalance: Chemical messengers that regulate gut function may be disrupted.
You might be interested: Functional Dyspepsia Treatment in Singapore
Types of IBS

IBS is often categorized into three main subtypes based on predominant stool patterns:
IBS with Constipation (IBS-C)
- Most stools are hard and lumpy
- Diagnosed when constipation is the predominant type of stool on at least 25% of days with abnormal bowel movements
- Symptoms include less frequent bowel movements, abdominal pain, and bloating
- May lead to straining during defecation and occasional bleeding when wiping
IBS with Diarrhea (IBS-D)
- Most stools are loose and watery
- Diagnosed when diarrhea is the predominant pattern on at least 25% of days with abnormal bowel movements
- Associated with increased frequency of bowel movements, cramp-like abdominal pain, bloating, and gas
You might want to read this: Celiac Disease Treatment in Singapore
IBS with Mixed Bowel Habits (IBS-M)
- Experience both hard/lumpy and loose/watery stools on the same day
- Alternates between periods of constipation and diarrhea
- Both constipation and diarrhea occur on at least 25% of days with abnormal bowel movements
If symptoms don’t fit these categories, the condition may be classified as IBS-Unspecified (IBS-U).
Common Symptoms of IBS
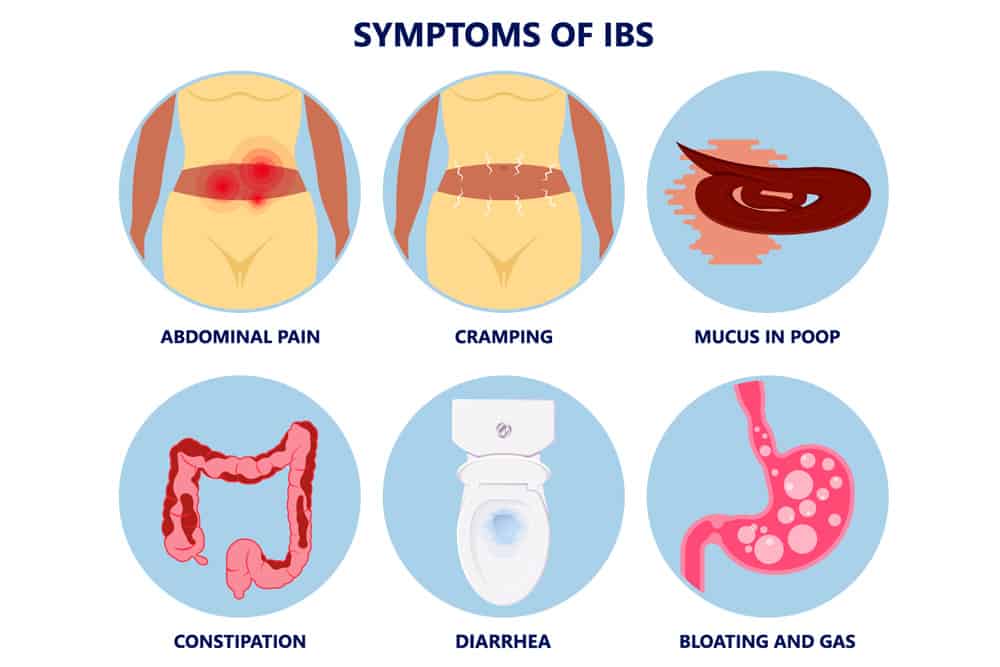
The symptoms of IBS can vary significantly between individuals and may change over time. Common symptoms include:
- Abdominal cramps or pain, typically occurring after meals and sometimes relieved after a bowel movement
- Bloating and gas
- Diarrhea, constipation, or alternating between both
- Altered appearance of stools (may contain mucus)
- Sensation of incomplete emptying after a bowel movement
- Increased frequency of bowel movements or flatulence
- Lethargy and fatigue
Some patients with IBS also experience non-gastrointestinal symptoms such as fatigue, muscle pain, sexual dysfunction, and sleep disturbances.
Red Flag Indicators
While IBS itself is not dangerous, certain symptoms should prompt immediate medical attention as they may indicate more serious conditions:
- Blood in stools (not a symptom of IBS)
- Age of onset over 60
- Unexplained, unintentional weight loss
- Family history of bowel or ovarian cancer
- Abdominal, rectal, or pelvic masses
- Anemia
- Elevated inflammatory markers
- Fever and chills
- Night sweats
- Difficulty swallowing
- Progressively worsening symptoms
Related article: The Ultimate Guide to Losing Weight in Singapore
Common Triggers for IBS
Understanding and managing triggers is crucial for IBS management. Common triggers include:
Food Triggers
Many patients identify food as a significant trigger for their symptoms.
While there is no universal diet that cures IBS, certain foods often play a role in symptom development, particularly when bloating, discomfort, and diarrhea are the main concerns.
For IBS-C (Constipation), common triggers include:
- Refined grain products instead of whole grains
- Processed foods like chips and cookies
- Coffee, carbonated beverages, and alcohol
- High-protein diets
- Dairy products and cheese
For IBS-D (Diarrhea), common triggers include:
- Excessive insoluble fiber (found in fruit and vegetable skins)
- Chocolate, alcohol, caffeine
- Foods containing fructose or sorbitol
- Carbonated beverages
- Large meals
- Fried or greasy foods
- Dairy products (for those with lactose intolerance)
- Gluten (for those with sensitivity)
Stress and Anxiety
Psychological factors can significantly affect IBS symptoms. Stress and anxiety can exacerbate symptoms due to the brain’s reduced ability to manage the body’s reaction to stress.
Medications
Several medications can trigger or worsen IBS symptoms:
- Antibiotics
- Some antidepressants
- Diabetic medications
- Cough medicines containing sorbitol
This might help: Homeopathy in Singapore
Menstruation
For women, IBS symptoms often worsen during menstruation due to hormonal fluctuations.
Other Factors
- Eating while distracted (such as while driving)
- Consuming food too quickly
- Insufficient physical activity
- Gastrointestinal infections (like food poisoning)
Diagnosis of IBS
IBS is primarily a clinical diagnosis based on symptoms and the exclusion of other conditions. The diagnostic process typically involves:
Medical History
A comprehensive medical history is crucial for accurate diagnosis. Doctors will ask about:
- Description of symptoms and their patterns
- Duration of symptoms (typically present weekly for about 6 months)
- Changes in bowel movement frequency
- Changes in stool appearance
- Presence of other symptoms like anemia or weight loss
- Personal and family history of gastrointestinal diseases
- Stressful events and experiences
- Dietary habits
Physical Examination
The doctor will check for:
- Abdominal bloating
- Sounds within the abdomen
- Tenderness or pain in the abdomen
Related article: Health Screening in Singapore
Diagnostic Criteria
The Rome IV criteria are commonly used for diagnosis (though primarily for research purposes). These criteria include:
- Recurrent abdominal pain occurring at least one day per week in the last three months, associated with two or more of the following:
- Related to defecation
- Associated with a change in stool frequency
- Associated with a change in stool form/appearance
- Symptoms should be present for the last 3 months with symptom onset at least 6 months prior to diagnosis
Diagnostic Tests
Depending on age and the presence of alarm symptoms, some patients may require additional testing to exclude other conditions:
- Blood tests for anemia, infections, and inflammation
- Stool tests for blood, infections, or inflammation
- Hydrogen breath test for bacterial overgrowth or lactose/fructose intolerance
- Upper gastrointestinal endoscopy and biopsy to check for celiac disease
- Colonoscopy to check for inflammatory bowel disease or colorectal cancer
- Imaging studies like X-rays, MRI, or CT scans in some cases
It’s important to note that the absence of findings on scans or endoscopy does not necessarily indicate the need for further testing, as IBS is a functional disorder without structural abnormalities.
Read more: Comprehensive Guide to Colonoscopy in Singapore
Management and Treatment of IBS
As IBS is a lifelong condition with no definitive cure, management focuses on symptom control and improving quality of life.
A personalized, multi-faceted approach is essential.
Lifestyle Modifications
- Regular Exercise: Physical activity helps regulate bowel function and reduce stress
- Stress Management: Techniques like deep breathing, meditation, and yoga can help manage symptoms
- Adequate Sleep: Poor sleep can exacerbate IBS symptoms
- Symptom Diary: Keeping track of symptoms and potential triggers helps identify patterns
- Proper Toilet Positioning: This can help with bowel movements
Dietary Approaches
- Low-FODMAP Diet: This involves avoiding certain carbohydrates that are poorly absorbed by the small intestine and ferment in the large intestine, producing gas. FODMAPs include:
- Fructose (fruits, honey, high-fructose corn syrup)
- Lactose (dairy products)
- Fructans (wheat, onions, garlic)
- Galactans (legumes)
- Polyols (sugar alcohols)
- Fiber Modification:
- For IBS-C: Gradually increase fiber intake to 25g (women) or 38g (men) daily through whole grains, legumes, fruits, and vegetables
- For IBS-D: Focus on soluble fiber in moderation (found in oats, barley, and some fruits)
- Other Dietary Strategies:
- Eat smaller, more frequent meals
- Drink plenty of water
- Avoid known trigger foods
- Consider gluten avoidance if sensitive
- Avoid extreme temperature foods in the same meal
Medications
Several medications may help manage specific IBS symptoms:
- For Diarrhea:
- Anti-diarrheals (e.g., loperamide)
- For Abdominal Pain and Spasms:
- Antispasmodics (e.g., mebeverine, alverine citrate, hyoscine)
- Peppermint oil
- For Constipation:
- Laxatives (e.g., polyethylene glycol, lactulose)
- Newer secretagogues for patients with constipation and abdominal pain
- Other Medications:
- Specific antibiotics for bacterial overgrowth
- Neuromodulators to reduce visceral sensitivity
- Prokinetics to help with incomplete bowel movements
- Supplements:
- Certain probiotics may help with bloating, gas, and diarrhea, though evidence varies
- Prebiotics and fiber supplements in some cases
Living with IBS in Singapore
In Singapore, approximately 10% of the population suffers from IBS, with the condition being more common in women.
Most people develop IBS in their 30s and 40s, though it can occur at any age.
Active self-management is crucial for individuals with IBS. Patients are encouraged to:
- Learn how to monitor their symptoms
- Rely on self-help measures during symptom flares
- Identify specific triggers
- Make informed dietary and lifestyle adjustments
For mild IBS symptoms, treatment can often be managed through primary care physicians at polyclinics or GP clinics.
However, patients with more complex or severe symptoms may benefit from referral to a gastroenterologist.
With proper diagnosis, explanation, and a personalized treatment plan, studies suggest that as many as 85% of patients can become largely symptom-free within a period of up to 6 months.
FAQs
What is the difference between IBS and IBD?
IBS (Irritable Bowel Syndrome) should not be confused with IBD (Inflammatory Bowel Disease).
IBS is a functional disorder with no visible inflammation or structural changes in the intestines, while IBD includes conditions like Crohn’s disease and ulcerative colitis, which involve chronic inflammation, tissue damage, and sometimes serious complications.
IBD typically requires different treatment approaches and may have more severe health implications than IBS.
Can dairy cause IBS symptoms?
Dairy products may trigger IBS symptoms in some individuals, especially if the dairy product is high in fat or if the person has lactose intolerance. Many people with IBS find that switching to low-fat or lactose-free dairy products can help alleviate symptoms. However, dairy is not a universal trigger for everyone with IBS, and some people can consume dairy without issues.
Is the low FODMAP diet effective for all IBS patients?
The low FODMAP diet has shown effectiveness for many IBS patients, particularly those suffering from bloating, gas, and diarrhea. However, it’s not a one-size-fits-all solution.
The diet works by restricting fermentable sugars found in certain foods that can cause symptoms in sensitive individuals.
While studies show it can improve symptoms in 50-80% of IBS patients, it’s meant to be a temporary elimination diet followed by careful reintroduction of foods.
The diet should be implemented under professional guidance, as it can be nutritionally restrictive if followed long-term.
How do I tell the difference between IBS and more serious conditions?
Several gastrointestinal diseases can mimic IBS symptoms, including celiac disease, inflammatory bowel disease, and colorectal cancer.
“Red flag” symptoms that suggest a condition other than IBS include blood in stools, unexplained weight loss, symptoms that begin after age 50, fever, anemia, and family history of colon cancer or inflammatory bowel disease.
If you experience any of these symptoms, seek medical attention promptly.
Proper diagnosis often involves excluding other conditions through tests like blood work, stool analysis, endoscopy, or colonoscopy.
Can stress management techniques really help with IBS?
Yes, stress management techniques can significantly help manage IBS symptoms for many patients. The brain-gut connection plays a crucial role in IBS, with stress and anxiety often triggering or worsening symptoms.
Various stress reduction methods have shown effectiveness, including cognitive behavioral therapy, mindfulness meditation, progressive muscle relaxation, and regular exercise.
These approaches help regulate the body’s stress response, which can directly influence gut function and pain perception.
While stress management alone may not completely resolve all IBS symptoms, it’s an important component of a comprehensive treatment plan.
Are probiotics helpful for IBS treatment?
The evidence for probiotics in IBS treatment is mixed. Some specific probiotic strains have shown benefit in reducing symptoms like bloating, gas, and diarrhea in certain patients.
However, not all probiotics are created equal, and the majority of over-the-counter probiotics have not been tested specifically for IBS treatment.
Some may even worsen symptoms like diarrhea and bloating.
If considering probiotics, it’s best to consult with a healthcare provider who can recommend specific strains with evidence behind them, rather than randomly selecting products off the shelf.
How long does IBS typically last?
IBS is generally considered a chronic, long-term condition that may persist throughout a person’s lifetime.
However, the severity and frequency of symptoms often fluctuate over time. Many people experience periods of remission with minimal symptoms alternating with flare-ups.
With appropriate management strategies, including dietary modifications, stress management, and sometimes medication, most people can effectively control their symptoms and maintain a good quality of life.
Studies suggest that with proper treatment plans, a significant percentage of patients can achieve substantial symptom relief within 6 months.
Is IBS more common in certain ethnicities in Singapore?
The available data doesn’t clearly indicate whether IBS affects certain ethnic groups in Singapore more than others.
IBS affects approximately 10% of Singapore’s population overall, which is somewhat lower than rates in Western countries.
The condition appears to be influenced more by gender (affecting more women than men) and age (typically affecting adults in their 30s and 40s) rather than ethnicity.
However, cultural differences in diet, stress levels, and healthcare-seeking behavior may influence how IBS presents and is diagnosed across different ethnic groups in Singapore’s multicultural society.
Can children develop IBS?
Yes, children can develop IBS, although it’s more commonly diagnosed in adults. The diagnostic criteria for children are similar but adapted for their age.
Children with IBS typically experience abdominal pain related to bowel movements, along with changes in stool frequency or appearance.
The condition can affect school attendance and social activities. Treatment approaches for children with IBS focus on education, dietary modifications, and sometimes psychological support.
If a child shows persistent abdominal pain, changes in bowel habits, or growth concerns, parents should consult a pediatrician who may refer to a pediatric gastroenterologist if needed.
What new treatments are being developed for IBS?
Research into new IBS treatments continues to evolve. Some promising areas include targeted medications that address specific symptoms, like new classes of drugs for visceral pain, gut motility issues, and microbiome modification.
Gut-directed hypnotherapy has shown effectiveness in clinical trials. Fecal microbiota transplantation is being researched for certain IBS subtypes, though evidence remains preliminary.
Digital therapeutics, including specialized apps for IBS management, are also emerging. While no breakthrough cure is on the horizon, these approaches aim to provide better symptom control and quality of life for people with IBS.

