As we age, maintaining good oral health becomes increasingly challenging yet remains vital for overall well-being.
Elderly individuals face unique dental challenges due to factors like aging tissues, medications, chronic health conditions, and sometimes limited dexterity. This comprehensive guide explores the most common dental problems affecting older adults, their symptoms, prevention strategies, and treatment options.
Why Dental Health Matters More in Your Senior Years
The enamel protecting our teeth is the toughest tissue in the human body, but decades of chewing, grinding, and exposure to chemicals and bacteria inevitably take their toll. For seniors, dental health isn’t just about maintaining a beautiful smile—it directly impacts nutrition, comfort, and quality of life.
Poor oral health can lead to:
- Difficulty eating and inadequate nutrition
- Increased risk of systemic diseases
- Pain and discomfort
- Social isolation and decreased self-confidence
- Complications with existing health conditions
7 Early Warning Signs of Dental Problems in the Elderly
Recognizing these early symptoms can help address dental issues before they become severe:
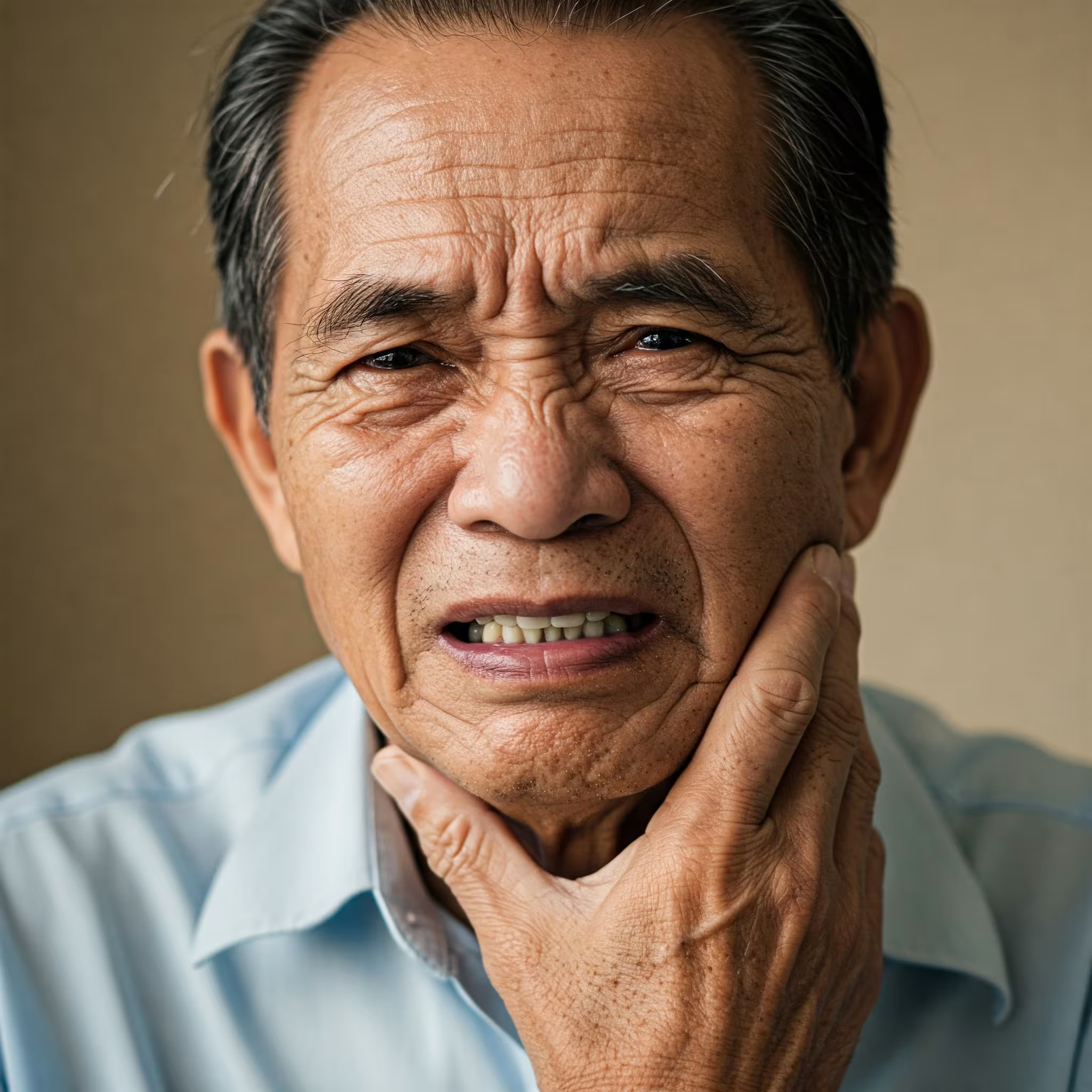
1. Toothache
Dental pain remains one of the primary reasons elderly patients visit dentists. Toothache refers to pain in and around the teeth and jaws and often signals tooth decay. If left untreated, decay can progress to an abscess (a collection of pus), causing inflammation in the gum, near teeth, or in the pulp. In severe cases, these infections can spread, becoming potentially life-threatening.
2. Sensitive Teeth
If your teeth hurt when consuming hot or cold food and beverages, you may have sensitive teeth. This sensitivity often results from:
- Tooth decay
- Fractured teeth
- Worn fillings
- Gum disease
- Worn tooth enamel
- Exposed tooth roots due to gum recession
The appropriate treatment depends on identifying the underlying cause of sensitivity. Consult a dentist promptly for proper diagnosis and treatment.
3. Bleeding or Sore Gums
Many older adults suffer from gum (periodontal) disease caused by bacteria in plaque that irritate the gums, making them sore, raw, and prone to bleeding. This initially leads to gingivitis—inflammation of the gums. When you have gingivitis, your gums can become painful, swollen, and bleed during brushing.
4. Mouth Sores
Mouth sores or canker sores (aphthous ulcers) are small, shallow lesions that appear on the soft tissues of the mouth or at the base of the gums. While not contagious, they can be unpleasant and make eating and talking difficult. In some cases, persistent mouth sores may indicate mouth cancer, which begins in the cells lining the mouth and can spread to the tongue, cheeks, roof of the mouth, lips, or gums.
5. Bad Breath
Also known as halitosis, persistent bad breath can result from poor dental hygiene, certain foods, or underlying health conditions. For many seniors, it can cause embarrassment and social anxiety. Bad breath is also a common symptom of denture stomatitis (inflammation of mouth tissues under dentures) or gum disease.
Seniors who wear dentures may experience bad breath due to improper cleaning or fit. Denture stomatitis is typically caused by a yeast or fungus called candida. Proper denture care and regular cleaning according to a dental professional’s instructions are essential.
6. Jaw Pain or Popping
These symptoms can have multiple causes, making diagnosis challenging. Possible culprits include:
- Sinus issues
- Toothache
- Inflammation
- Infection
- Teeth grinding (bruxism)
- Gingivitis
- Temporomandibular joint (TMJ) disorders
A thorough examination by a dentist, potentially including X-rays, is necessary to determine the exact cause and appropriate treatment.
7. Cracked or Broken Teeth
Teeth can crack or break due to brittle teeth, grinding, or injury. Some cracks may be invisible to the naked eye and even to X-rays, but if left untreated, they can cause significant pain and lead to more serious problems. Seek dental attention if you experience discomfort when chewing.
Common Dental Problems in the Elderly
Dry Mouth (Xerostomia)
Affecting approximately 30% of people over 65, dry mouth occurs when salivary glands don’t produce enough saliva. This condition leads to oral discomfort and significantly increases the risk of tooth decay.
- Medication side effects (antihypertensives, diuretics, antihistamines, opioids)
- Systemic diseases
- Cancer treatments
- Age-related changes in salivary function
Symptoms range from:
- Difficulty chewing and swallowing
- Persistent sticky feeling in the mouth
- Increased thirst
- Burning sensation in the mouth
- Cracked lips
- Mouth sores
Left untreated, dry mouth can dramatically impact oral health and quality of life, making it crucial to address promptly.
Gum Disease (Periodontitis)
Gum disease affects nearly 60% of adults aged 65 and older. This inflammatory condition can significantly impact overall health and quality of life, potentially leading to tooth loss and difficulty eating.
Risk factors include:
- Decreased self-care ability
- Multiple chronic conditions
- Limited access to affordable dental care
- Smoking
- Diabetes
- Poor oral hygiene
Studies show that gum disease in elderly patients is associated with systemic issues like diabetes and cardiovascular disease, highlighting the connection between oral health and general health.
Tooth Loss
Tooth loss remains one of the most significant consequences of poor oral health in the elderly. According to data from nursing homes, approximately 25% of older adults have complete tooth loss, while 66% experience partial tooth loss.
The impacts extend beyond cosmetic concerns:
- Poor nutrition due to difficulty chewing
- Increased risk of chronic diseases
- Decreased self-esteem and social confidence
- Speech difficulties
The National Institute of Dental and Craniofacial Research reports that seniors aged 65 and older have an average of 20.7 remaining teeth (out of 32), with factors like age, smoking history, and socioeconomic status influencing tooth loss rates.
Tooth Decay (Dental Caries)
Dental caries remain highly prevalent among seniors, with the American Dental Association reporting that about 18% of adults aged 65 and older have untreated cavities.
Key risk factors for elderly tooth decay include:
- Gum recession exposing vulnerable root surfaces
- Medication-induced dry mouth
- Cognitive and physical impairments affecting oral hygiene
- Reduced fluoride exposure
- Diet high in sugars and carbohydrates
Studies show that the total prevalence of dental caries in seniors increased from 93% to 96.2% between 1999-2004 and 2011-2016, highlighting growing concerns about elderly oral health.
Root Caries
Root caries are particularly common in older adults due to gum recession that exposes the tooth roots. Unlike the crown of the tooth, roots lack protective enamel and are more vulnerable to decay when exposed to acids and bacteria.
Denture-Related Issues
Many seniors replace missing teeth with full or partial dentures. Prolonged denture use can cause:
- Inflammation of oral tissues (stomatitis)
- Yeast infections (candidiasis)
- Bone loss in the jaw
- Sore spots and ulcers
- Difficulty eating and speaking
Oral Cancer
The risk of oral cancer increases significantly after age 50, especially for those who use tobacco products. Men are approximately three times more likely to develop oral cancer than women. Regular dental check-ups are crucial for early detection, as early-stage oral cancer often produces no noticeable symptoms.
The Connection Between Oral Health and Overall Health
Poor oral health can have far-reaching consequences beyond the mouth. For elderly individuals, dental problems can impact:
Nutrition
- Loose teeth, toothaches, or missing teeth make chewing uncomfortable
- Reduced chewing efficiency leads to dietary restrictions
- Limited food choices may result in nutritional deficiencies
Systemic Health Conditions
- Periodontal disease has been linked to diabetes and cardiovascular issues
- Bacteria from oral infections can enter the bloodstream
- Chronic inflammation in the mouth may contribute to inflammation elsewhere in the body
Quality of Life
- Dental issues can negatively affect self-esteem and social interactions
- Pain and discomfort can disrupt daily activities and sleep
- Communication difficulties may lead to social isolation
Prevention and Maintenance of Good Oral Health
Regular Dental Visits
Seniors should visit the dentist at least twice a year for professional cleanings and check-ups. These visits allow for:
- Early detection of potential problems
- Professional removal of plaque and tartar
- Assessment of denture fit and condition
- Screening for oral cancer
- Personalized advice for home care
Daily Oral Hygiene Practices
1. Brushing
- Brush teeth at least twice daily with fluoride toothpaste
- Use a soft-bristled toothbrush to avoid damaging gums and enamel
- For those with arthritis or limited dexterity:
- Consider using an electric toothbrush
- Enlarge the toothbrush handle by wrapping a sponge around it
- Try adaptive devices designed for those with grip difficulties
2. Flossing
- Floss at least once daily to remove plaque between teeth
- Consider floss holders or water flossers if traditional flossing is difficult
- Interdental brushes may be easier to use for some seniors
3. Mouthwash
- Use an alcohol-free antimicrobial mouthwash to reduce plaque
- Consider fluoride rinses to strengthen enamel and prevent decay
- For dry mouth, specialized moisturizing mouth rinses are available
4. Denture Care
- Remove dentures at night to allow tissues to rest
- Clean dentures daily according to professional instructions
- Soak dentures in appropriate cleaning solution
- Check regularly for proper fit and wear
- Schedule professional denture adjustments when needed
Diet and Lifestyle Factors
- Stay well-hydrated to promote adequate saliva production
- Limit sugary foods and beverages that feed decay-causing bacteria
- Eat a balanced diet rich in calcium, phosphorus, and vitamin D for tooth strength
- Avoid tobacco products and excessive alcohol consumption
- Manage chronic conditions like diabetes that impact oral health
Dental Care Solutions for the Elderly
Adaptive Tools and Technologies
- Electric toothbrushes with pressure sensors and timers
- Water flossers for easier interdental cleaning
- Toothbrush adaptations for those with dexterity issues
- High-fluoride toothpastes prescribed for high-risk patients
Denture Alternatives
Modern dentistry offers several options beyond traditional dentures:
Implant-Supported Dentures
Also known as “clip-on teeth,” these combine dentures with dental implants—titanium posts surgically placed in the jawbone. Benefits include:
- Greater stability and security
- Improved chewing efficiency
- Prevention of bone loss
- Reduced gum irritation and sore spots
- No need for denture adhesives
Dental Implants
For replacing individual teeth, dental implants provide a permanent solution that:
- Look and function like natural teeth
- Prevent bone loss
- Don’t require altering adjacent teeth
- Can last a lifetime with proper care
Read more: The Ultimate Guide to Dental Implants in Singapore
Specialized Care for Those with Limited Mobility
For elderly individuals who cannot easily visit a dental office, options include:
- Mobile dental services that come to homes or care facilities
- Special equipment for treating patients who cannot transfer to a dental chair
- Teledentistry for remote consultations and monitoring
Tips for Caregivers
If you’re caring for an elderly person, watch for these warning signs of dental problems:
- Avoiding one side of the mouth when eating
- Refusing previously enjoyed foods
- Persistent bad breath
- Red, swollen gums that bleed during brushing
- Visibly longer teeth (due to receding gums)
- Loose or broken teeth
- White patches or ulcers that don’t heal
Caregivers may need to assist with daily oral hygiene, especially for those with dementia or physical limitations. This includes:
- Gentle reminders about brushing and flossing
- Physical assistance with holding dental tools
- Regular denture cleaning
- Scheduling and transportation to dental appointments
- Monitoring for signs of discomfort or problems
FAQ: Common Elderly Dental Problems
How often should elderly adults visit the dentist?
Seniors should visit the dentist at least twice a year for check-ups and professional cleanings. Those with existing dental issues or chronic conditions like diabetes may need more frequent visits, as recommended by their dentist.
How often should an elderly adult have their teeth professionally cleaned?
Elderly adults should maintain a 6-month cleaning schedule with their dental hygienist, as they are more susceptible to conditions like gum disease and dry mouth. Some patients with advanced periodontal disease may benefit from cleanings every 3-4 months.
At what age do gums typically start to recede?
Gum recession can begin at any age due to factors like aggressive brushing, periodontal disease, or genetics. However, it becomes significantly more common after age 65, affecting a large percentage of seniors.
What is the most common geriatric dental problem?
Periodontal (gum) disease and dental caries, especially root caries, are among the most prevalent dental problems in geriatric patients. Dry mouth, which increases the risk of both these conditions, is also extremely common.
How does aging affect oral health?
Aging brings several changes to oral health, including:
- Decreased temporomandibular joint movement
- Thinning of tooth enamel
- Reduced saliva production
- Decreased cell renewal in oral tissues
- Receding gums exposing tooth roots
- These changes can affect speech, chewing ability, taste sensation, and masticatory efficiency, which may decrease by 15-16%.
How can seniors with arthritis manage their oral hygiene?
Seniors with arthritis can:
- Use electric toothbrushes that require less manual dexterity
- Modify toothbrushes with larger handles or grip attachments
- Consider water flossers instead of traditional floss
- Use toothpaste dispensers and other adaptive devices
- Ask for assistance from caregivers when necessary
Should seniors with no natural teeth still visit the dentist?
Yes, absolutely. Regular dental visits remain important even for those with complete tooth loss. Dentists check for proper denture fit, oral cancer, tissue inflammation, fungal infections, and other oral health issues that affect quality of life.
How does dry mouth affect dental health in seniors?
Dry mouth (xerostomia) significantly increases the risk of tooth decay, gum disease, and oral infections. Without adequate saliva to neutralize acids and wash away food particles, bacteria thrive. Dry mouth can also make speaking and swallowing difficult and affect taste perception.
What dental care options exist for homebound seniors?
Homebound seniors have several options:
- Mobile dental services that provide care at home
- Teledentistry for remote consultations and monitoring
- Caregiver-assisted daily oral hygiene
- Coordination with primary care providers for basic oral health assessments
How do medications affect oral health in the elderly?
Many medications commonly prescribed to seniors cause dry mouth, including antihypertensives, antidepressants, diuretics, antihistamines, and pain medications. Some medications can also cause gum overgrowth, taste alterations, or oral infections. Always inform your dentist about all medications you’re taking.
Can lost teeth affect nutrition in elderly patients?
Yes, tooth loss significantly impacts nutrition. Missing teeth reduce chewing efficiency, often leading seniors to avoid nutritious but harder-to-chew foods like fruits, vegetables, and proteins. This can result in nutritional deficiencies and related health problems. Proper tooth replacement through dentures or implants helps maintain proper nutrition.
Conclusion
As we age, maintaining good oral health becomes increasingly important yet challenging. Understanding the common dental issues faced by older adults allows for proactive prevention and timely intervention. Regular dental check-ups, proper daily hygiene practices, and a healthy diet are crucial in preventing and managing conditions like dry mouth, gum disease, and tooth decay.
Remember that oral health is closely linked to overall well-being. Don’t hesitate to discuss any concerns with your dentist, who can provide personalized advice and treatment options. With the right care and attention, you can preserve your smile and enjoy optimal dental health well into your golden years.
The importance of dental care rises in later life. Cultivating good oral hygiene habits reduces the chances of dental and other health issues, enhancing quality of life and supporting overall health during the senior years.