Sleep apnea is a concerning condition that affects both adults and children, characterized by disruptions in breathing during sleep.
In children specifically, paediatric sleep apnea occurs when the upper airway becomes too narrow due to tissue swelling, anatomical obstruction, or excessive floppiness.
This results in a disrupted oxygen supply and leads to poor, disturbed sleep with significant short and long-term consequences for a child’s health and development.
In Singapore, paediatric sleep apnea is more common than many parents realize, yet it remains under-diagnosed.
This comprehensive guide aims to provide parents, caregivers, and healthcare providers with essential information about paediatric sleep apnea, its symptoms, diagnosis, treatment options available in Singapore, and its potential impact on a child’s well-being and growth.
Understanding Paediatric Sleep Apnea
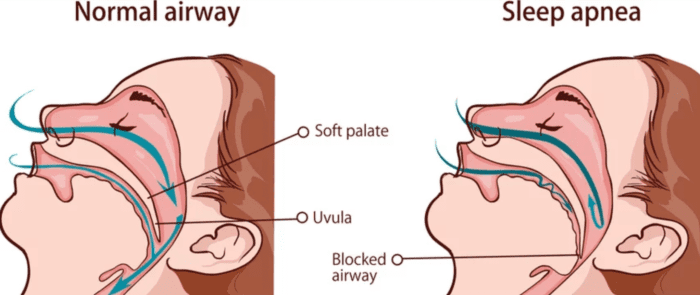
Paediatric sleep apnea simply refers to sleep apnea that occurs in children. When a child has a very small airway, it can collapse or become obstructed during sleep.
This results in the child receiving a disrupted supply of oxygen, which often leads to a night of poor, fragmented sleep.
Unlike adult sleep apnea, where patients can articulate that they feel tired or have unrefreshed sleep, children often cannot express these symptoms.
Instead, the condition manifests through various behavioral, cognitive, and physical symptoms that parents might not immediately associate with sleep problems.
Read more: Which ENT Doctor in Singapore Should You Consider?
The Difference Between Snoring and Sleep Apnea
It’s crucial for parents to understand that not all snoring indicates sleep apnea, but all children who snore regularly should be assessed for sleep apnea:
- Snoring occurs when the airway vibrates as a result of some narrowing. It signifies that there is some obstruction in the airway. A child can snore without having sleep apnea, but any child who snores regularly (3 or more nights per week) needs evaluation.
- Sleep apnea typically presents with snoring plus disturbed, restless sleep. In some cases, the child may not snore prominently because their airway keeps getting blocked, resulting in breathing pauses or choking. Children with sleep apnea may sleep with their head tilted upward and mouth open to naturally open the airway.
Prevalence and Risk Factors
Paediatric sleep apnea affects both boys and girls equally, with two distinct peak periods:
- First peak: Between ages 2-8 years, coinciding with the period when lymphoid hyperplasia and adenotonsillar hypertrophy are most common
- Second peak: In older children and adolescents who are typically obese
Risk Factors for Paediatric Sleep Apnea
Several factors increase a child’s risk of developing sleep apnea.
The most common cause in children is enlarged tonsils and adenoids, followed by obesity (particularly relevant for older children and adolescents).
Children with allergic rhinitis often experience nasal congestion and airway narrowing that contributes to sleep apnea.
Craniofacial abnormalities, including small jaw (micrognathia) and midface hypoplasia, can significantly impact airway dimensions.
Neuromuscular disorders such as muscular dystrophies and cerebral palsy affect muscle tone in the upper airway.
Genetic conditions including Down syndrome (Trisomy 21), Prader-Willi Syndrome, and Achondroplasia (short-limbed dwarfism) are strongly associated with sleep apnea risk.
Family history of sleep and breathing disorders also increases a child’s predisposition.
Children with these risk factors should be monitored more closely for signs of sleep apnea, as early intervention can prevent long-term complications.
Signs and Symptoms of Paediatric Sleep Apnea
Identifying sleep apnea in children can be challenging as symptoms may not be immediately obvious. Parents should be aware of both nighttime and daytime signs.
Nighttime Symptoms
Children with sleep apnea typically exhibit habitual loud snoring and disturbed, restless sleep.
Parents may notice labored breathing during sleep, with occasional breathing pauses, gasping, or choking sounds.
Many children adopt unusual sleeping positions (such as frog-like posture, tilted chin, or head off the bed) to naturally keep their airways open.
Excessive sweating during sleep, frequent awakenings, nightmares or night terrors, and bedwetting (enuresis) are common.
Mouth breathing during sleep is also frequently observed as children attempt to increase airflow.
Daytime Symptoms
During waking hours, children with sleep apnea often experience daytime sleepiness or difficulty waking up in the morning.
Morning headaches are common due to nighttime oxygen fluctuations. Many children appear to have unrefreshed sleep despite adequate time in bed.
Behavioral manifestations include irritability, aggression, or moodiness, hyperactivity issues, attention problems or poor concentration, and various behavioral difficulties.
Academic performance typically suffers, with children sometimes falling asleep in school or at unusual times.
Physical Signs
Children with sleep apnea often develop a chronic mouth breathing posture, even during waking hours.
Physical examination may reveal swollen nasal tissue and enlarged tonsils and adenoids. Some children present with a small chin, which can contribute to airway narrowing.
Growth patterns may be affected, with some children showing poor growth or failure to thrive.
Weight issues can manifest on either extreme—some children may be underweight due to increased work of breathing, while others may be overweight or obese, which can further contribute to sleep apnea severity.
It’s important to note that some of these symptoms, particularly hyperactivity and attention problems, can mimic Attention Deficit Hyperactivity Disorder (ADHD).
In fact, studies suggest that some children diagnosed with ADHD might actually have undiagnosed sleep apnea.
Read more: ADHD Diagnosis in Singapore
How Paediatric Sleep Apnea Affects Your Child’s Health
Untreated sleep apnea can have significant and wide-ranging effects on a child’s health, development, and quality of life.
Impact on Sleep Quality
When the airway is obstructed, oxygen levels drop, causing stress to the body. This typically occurs during deep sleep or dream sleep when airways are most relaxed.
The drop in oxygen triggers the brain to wake the child or change sleep position, disrupting the natural sleep cycle.
These disruptions prevent children from getting adequate restorative sleep, leading to many of the daytime symptoms mentioned above.
Parents of children with sleep apnea often experience disrupted sleep themselves due to their child’s frequent awakenings or behavioral issues.
Related article: Insomnia Treatment in Singapore
Effects on Growth and Development
Growth hormone is primarily secreted during deep sleep. When a child’s airway is obstructed, it results in much lighter sleep and less secretion of growth hormone. This can lead to:
- Poor growth or weight gain
- Developmental delays
- Impaired facial growth and jaw development
Children who breathe through their mouths due to nasal obstruction often develop narrowed jaws and sometimes longer faces.
The narrowed jaws then predispose them to smaller airways as adults, potentially setting up a cycle of sleep-disordered breathing.
Related article: Eating Disorder Treatment in Singapore: Causes, Recovery
Cardiovascular Effects
Lowered oxygen levels can result in heart problems, as the heart must work harder when oxygen levels drop. This can lead to:
- Increased blood pressure
- Endothelial dysfunction
- Heart strain
- In rare cases, heart failure
As early as the 1960s, there were reports of children with heart failure whose condition reversed after removing their adenoids.
Even today, there are cases of children who develop heart failure as a result of large adenoids.
This might help: Which Cardiologist in Singapore Should You Consider? (Sort by Reviews)
Neurocognitive and Behavioral Impact
Sleep apnea significantly affects brain function and development in children, leading to:
- Reduced neurocognitive performance
- Learning difficulties
- Behavioral problems
- Mood disturbances
- Attention deficits
Many studies have shown that children with sleep apnea may not perform as well academically compared to children who breathe properly and have good sleep quality.
Related article: Autism Assessment in Singapore
Metabolic Effects
Untreated sleep apnea has also been associated with:
- Diabetes
- Obesity or difficulty maintaining healthy weight
- Metabolic syndrome
You might like: Diabetes Treatment in Singapore: Types, Risks
Diagnosis of Paediatric Sleep Apnea in Singapore
Proper diagnosis of sleep apnea is crucial for effective treatment. In Singapore, the diagnostic approach typically involves several steps.
When to Consult a Doctor
Parents should seek medical evaluation if they notice:
- Regular or habitual snoring (3 or more nights per week)
- Any of the nighttime or daytime symptoms mentioned above
- Physical signs suggesting upper airway obstruction
- Risk factors for sleep apnea
Initial Assessment
The first step usually involves consultation with a pediatrician or ENT specialist who will take a detailed history of snoring and sleep-related symptoms.
They will assess the child’s growth and development patterns over time and examine the upper airway, focusing on tonsil size, adenoid tissue, and nasal passages.
Healthcare providers will evaluate for features of atopy (allergic tendencies) and check for craniofacial abnormalities that might contribute to airway obstruction.
However, clinical history and physical examination alone are not sufficient to differentiate between simple snoring and obstructive sleep apnea.
Sleep Studies
The gold standard for diagnosing sleep apnea is polysomnography (PSG), a comprehensive sleep study.
In Singapore, this typically involves an overnight stay in a sleep laboratory with continuous monitoring of various parameters.
These include oronasal airflow, nasal pressure, electrocardiogram (ECG), electroencephalogram (EEG), oxygen saturation levels, chest and abdominal respiratory efforts, and muscle tone.
A dedicated paediatric sleep physician (usually a respiratory specialist with special training in performing sleep studies in children) interprets the results.
During the study, a caregiver is typically allowed to stay overnight with the child.
In Singapore, an inpatient sleep study typically costs between $2,000 and $3,000 in the private sector, with varying costs in public hospitals depending on the ward class chosen.
Alternative Diagnostic Methods
When full polysomnography is not available or practical, alternatives include:
- Overnight pulse oximetry: Can be done at home to monitor oxygen levels during sleep
- Home-based sleep studies: Less comprehensive but more convenient
However, these alternatives may miss episodes of airway obstruction that don’t cause significant oxygen desaturation.
A negative result doesn’t rule out sleep apnea if symptoms persist.
Treatment Options in Singapore
Treatment approaches for paediatric sleep apnea depend on the underlying cause, severity of the condition, and the child’s overall health.
In Singapore, several treatment options are available.
Surgical Interventions
Adenotonsillectomy
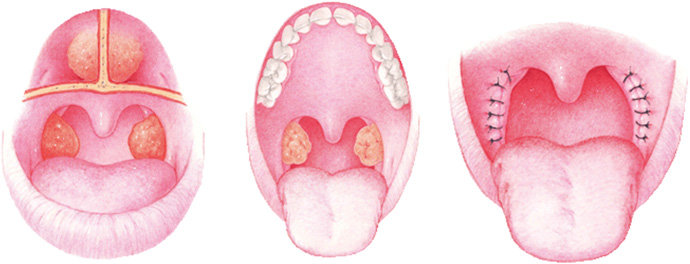
For children whose sleep apnea is primarily caused by enlarged tonsils and adenoids, surgical removal (adenotonsillectomy) is typically the first-line treatment.
The Childhood Adenotonsillectomy Trial (CHAT) showed that removing adenoids and tonsils improved symptoms, quality of life, and behavior in children with sleep apnea.
In Singapore, this procedure follows Ministry of Health (MOH) pricing guidelines and is partially claimable under MediSave, though it may not cover the entire cost, especially in private hospitals.
Post-surgery, close monitoring is essential as some children may have residual sleep apnea, particularly those with:
- Obesity
- Severe pre-surgery OSA
- Significant weight gain after surgery
- Down syndrome
- Neuromuscular weakness
- Craniofacial abnormalities
Other Surgical Options
In selected cases, additional or alternative surgical interventions may include:
- Nasal surgery to address the nasal valve area
- Palate surgery
- Tongue base procedures
- Facial advancement surgeries for children with craniofacial disproportions
Medical Management
Treatment of Nasal Allergies
For children with allergic rhinitis contributing to their sleep apnea, medical management may include:
- Nasal steroids
- Nasal saline douches
- Antihistamines
- Leukotriene receptor antagonists
- Allergen avoidance strategies
Continuous Positive Airway Pressure (CPAP)
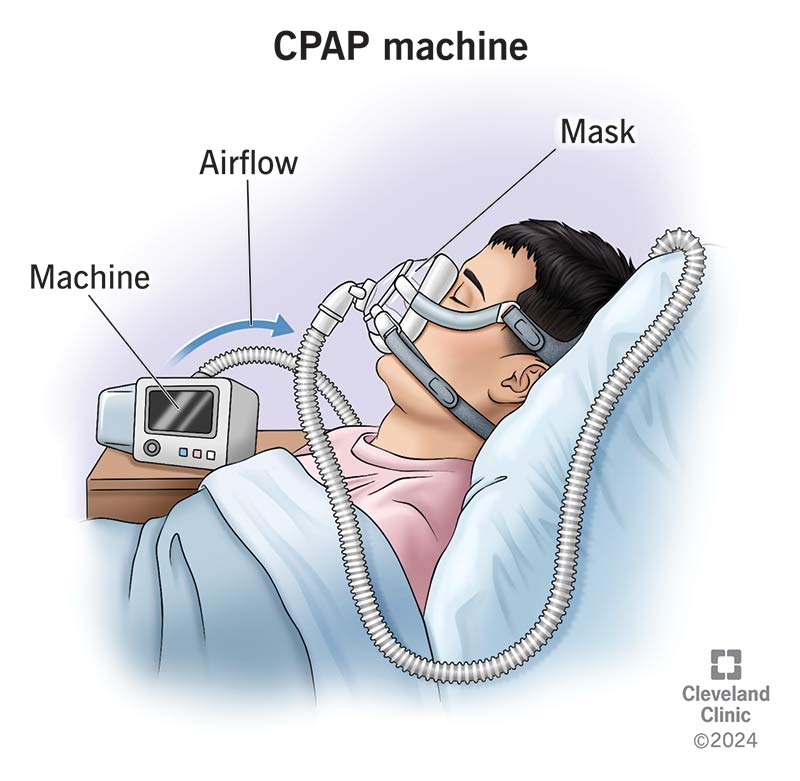
Unlike in adults where CPAP is often the first-line treatment, in children, CPAP is typically reserved for:
- Children with persistent sleep apnea despite surgery
- Cases where surgery is not an option
- Children with specific conditions making them unsuitable for surgery
The CPAP setup consists of a mask worn over the nose during sleep, connected by tubing to a machine that generates and delivers positive pressure to keep the airway open.
Adherence to CPAP can be challenging in children. In Singapore, a multidisciplinary team approach involving sleep specialists, sleep nurses, and child psychologists helps ensure proper usage and follow-up.
Orthodontic Interventions
In selected cases, orthodontic treatments may help address structural factors contributing to sleep apnea.
These include rapid maxillary expansion and palate expanders to widen the upper palate, which determines the lateral size of the airway.
Mandibular advancement devices are also utilized. These interventions are typically coordinated between dental specialists and sleep physicians.
Lifestyle Modifications
Weight Management
Weight management is crucial for obese children with sleep apnea.
Weight reduction strategies include dietary modifications, regular exercise programs, behavioral interventions, and referral to pediatric weight management programs.
Myofunctional Therapy
Myofunctional therapy involves exercises to increase muscle strength and tone in the upper airway.
While most data comes from adult studies, these exercises may benefit some children with sleep apnea.
MediSave Coverage in Singapore
In Singapore, treatment for pediatric sleep apnea is claimable under MediSave, though coverage varies.
MediSave can be used for sleep studies and surgical interventions; however, it typically doesn’t cover the whole cost of private-sector treatment.
Coverage for public hospitals depends on the ward class chosen.
Parents should consult with healthcare providers and hospital financial counselors to understand the costs and coverage options available.
Long-term Management and Follow-up
Managing paediatric sleep apnea is not just about immediate treatment but also long-term follow-up to ensure optimal outcomes.
Managing pediatric sleep apnea involves not just immediate treatment but also long-term follow-up to ensure optimal outcomes.
After initial treatment, children should be monitored for resolution of symptoms, improvement in sleep quality, growth and development, and possible residual sleep apnea.
In some cases, follow-up sleep studies may be recommended to confirm resolution of sleep apnea, especially in children with risk factors for residual disease.
Comprehensive management should also address any associated conditions, including learning or behavioral difficulties, growth issues, cardiovascular problems, and metabolic disorders.
As children grow, ongoing monitoring and management may be necessary, particularly for those with obesity, craniofacial abnormalities, neuromuscular disorders, or genetic syndromes.
Importance of Early Intervention
Early recognition and treatment of paediatric sleep apnea are crucial for several reasons:
- Preventing long-term complications
- Supporting normal growth and development
- Improving academic performance and behavior
- Enhancing quality of life for both child and family
- Preventing facial growth abnormalities that may predispose to adult sleep apnea
Remember that by age 4, children’s jaws are approximately 60% grown, and by age 12, they’re about 90% grown.
Early intervention for breathing issues can significantly impact facial development and future airway health.
Conclusion
Paediatric sleep apnea is a significant health concern that affects many children in Singapore.
Though often underdiagnosed, its impact on a child’s health, development, and quality of life can be substantial.
From poor school performance and behavioral issues to growth problems and cardiovascular concerns, the consequences of untreated sleep apnea extend far beyond just a poor night’s sleep.
With increased awareness, early recognition, proper diagnosis, and appropriate treatment, children with sleep apnea can achieve significant improvements in their symptoms and overall well-being.
In Singapore, various diagnostic and treatment options are available, with support from MediSave to help manage costs.
Parents who suspect their child may have sleep apnea should seek evaluation from appropriate healthcare providers.
Remember that being able to breathe well is essential to sleeping well and ultimately to living well.
Frequently Asked Questions
What is the difference between adult and paediatric sleep apnea?
Paediatric sleep apnea differs from adult sleep apnea in several key ways. In children, the most common cause is enlarged tonsils and adenoids, while in adults, obesity is the primary factor.
Children often present with hyperactivity and behavioral issues rather than daytime sleepiness that’s common in adults.
Additionally, children may exhibit growth problems, while adults typically don’t have this concern.
The approach to treatment also differs, with surgery (adenotonsillectomy) being the first-line treatment for children, whereas CPAP therapy is usually the primary intervention for adults.
At what age can children develop sleep apnea?
Children can develop sleep apnea at any age, including infancy.
However, there are two peak periods: the first between ages 2-8 years (coinciding with the period when adenotonsillar hypertrophy is most common) and the second in older children and adolescents who are typically obese.
Very young children under 2 years are less likely to snore, which can make sleep apnea harder to identify in this age group.
How is sleep apnea diagnosed in children who cannot cooperate with sleep studies?
For young children who may not cooperate with traditional sleep studies, modified approaches are used.
These include having a parent stay overnight during the study to provide comfort, using child-friendly equipment and environments, and sometimes using alternative diagnostic methods like overnight pulse oximetry at home.
Specialized pediatric sleep laboratories in Singapore are equipped to handle young children and make the experience as comfortable as possible.
Can my child outgrow sleep apnea?
Some children can outgrow sleep apnea, particularly if it’s related to enlarged tonsils and adenoids, as lymphoid tissue naturally reduces in size as children get older. However, children with obesity, craniofacial abnormalities, or certain genetic conditions may not outgrow the condition and might require ongoing management. Even after successful treatment, some children may experience a recurrence during growth spurts or if they develop obesity later in childhood.
How do I know if my child’s snoring is normal or a sign of sleep apnea?
While occasional snoring can be normal in children, habitual snoring (occurring 3 or more nights per week) warrants evaluation.
Signs that suggest your child’s snoring might be related to sleep apnea include: pauses in breathing followed by gasping or choking sounds, extremely restless sleep, unusual sleeping positions, excessive sweating during sleep, and daytime symptoms like hyperactivity, attention problems, or excessive tiredness.
If you notice these signs alongside snoring, consultation with a healthcare provider is recommended.
Will removing my child’s tonsils and adenoids cure their sleep apnea?
Adenotonsillectomy (removal of tonsils and adenoids) resolves sleep apnea in approximately 75-80% of otherwise healthy children with enlarged tonsils and adenoids.
However, some children may have residual sleep apnea even after surgery, particularly those with obesity, severe pre-surgery OSA, craniofacial abnormalities, neuromuscular disorders, or genetic syndromes like Down syndrome.
Follow-up evaluation after surgery is important to ensure the condition has resolved completely.
Can untreated sleep apnea affect my child’s IQ or learning abilities?
Yes, untreated sleep apnea can potentially impact a child’s cognitive development, learning abilities, and academic performance.
Studies have shown associations between sleep apnea and reduced attention span, impaired executive function, memory problems, and lower academic achievement.
The good news is that many of these cognitive effects can improve with appropriate treatment of the sleep apnea, highlighting the importance of early intervention.
Are there any natural remedies or lifestyle changes that can help with paediatric sleep apnea?
While natural remedies alone are usually not sufficient for treating moderate to severe sleep apnea, certain lifestyle modifications can help manage mild cases or complement medical treatment.
These include maintaining a healthy weight, treating allergies and nasal congestion, ensuring proper sleep hygiene and positioning, and in some cases, myofunctional therapy exercises to strengthen airway muscles.
However, these approaches should be discussed with and monitored by healthcare providers rather than used as sole treatments for diagnosed sleep apnea.
How long does recovery take after adenotonsillectomy in children?
Recovery after adenotonsillectomy typically takes about 7-14 days in children.
Most children experience throat pain, difficulty swallowing, and mild to moderate discomfort during this period. Pain medication and adequate hydration are important during recovery.
Improvements in sleep quality and breathing patterns are often noticed within days to weeks after surgery, though complete resolution of all symptoms may take longer.
Follow-up appointments are important to assess healing and symptom improvement.
Does MediSave cover all aspects of sleep apnea treatment in Singapore?
MediSave in Singapore can be used for sleep apnea diagnosis and treatment, but coverage varies.
It typically helps offset the cost of sleep studies and surgical procedures like adenotonsillectomy, but may not cover the entire expense, especially in private hospitals.
For ongoing treatments like CPAP therapy, additional equipment, or specialist consultations, coverage may be limited.
Families should consult with hospital financial counselors to understand specific coverage details and out-of-pocket expenses based on their situation and the healthcare setting (public vs. private).

