Constipation is one of the most common digestive complaints affecting people worldwide, with a particularly high prevalence in Singapore.
According to a study published in the Singapore Medical Journal, about 7.3% of Singaporeans aged 16 years and above experience constipation – significantly higher than the global average of around 2%.
While constipation is rarely life-threatening, it can cause considerable discomfort, frustration, and negatively impact quality of life if left untreated.
This comprehensive guide explores the causes, symptoms, and various treatment options available in Singapore for managing constipation effectively.
Understanding Constipation
What Is Constipation?
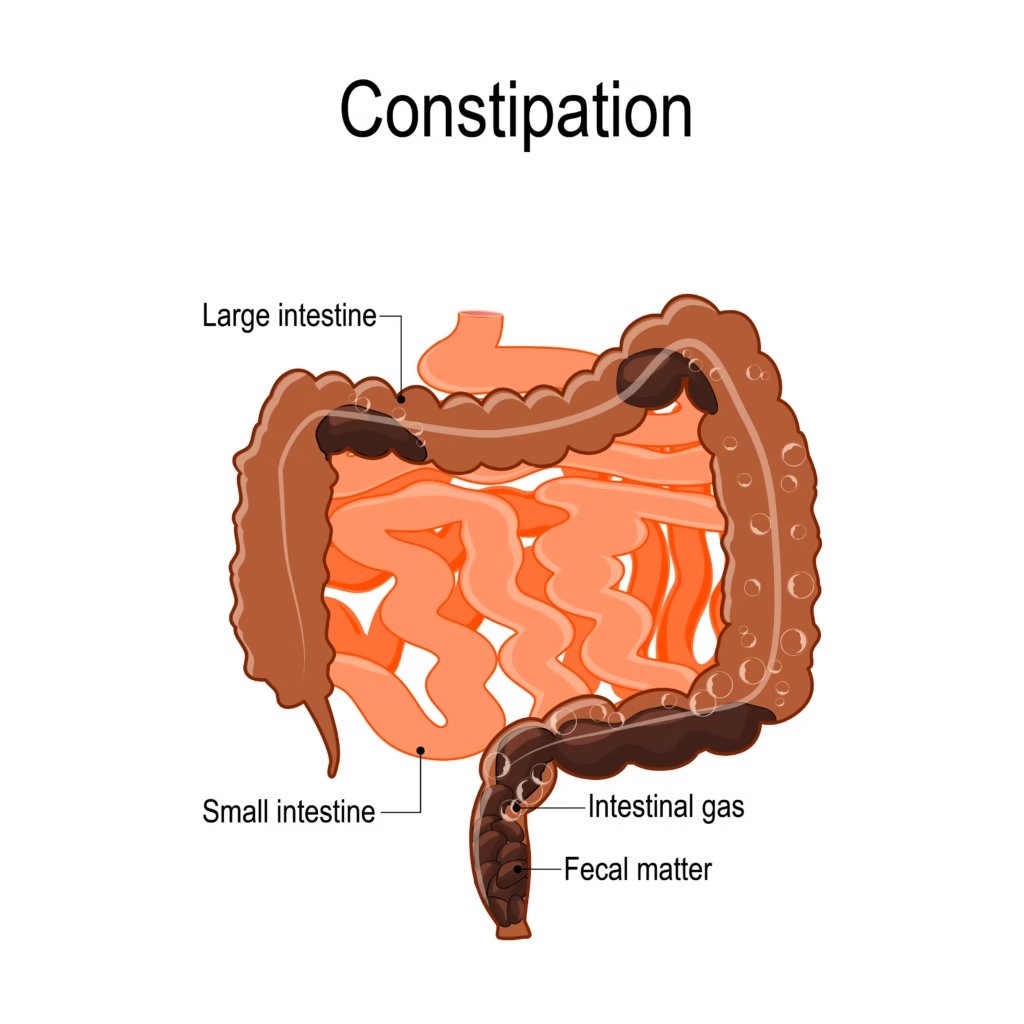
Constipation is generally described as difficulty or decrease in the frequency of passing stools. It occurs when bowel movements become difficult or less frequent than your normal pattern. The stools are usually hard and dry, making them difficult to pass.
It’s important to note that normal bowel movement patterns vary widely among individuals – ranging from three times a day to three times a week. You’re considered constipated when your pattern slows down noticeably, with hard stools that are difficult to pass.
According to medical guidelines, constipation is diagnosed when a person has two or fewer bowel movements in a week, or experiences at least two of the following symptoms for three months or longer:
- Straining during a bowel movement more than 25% of the time
- Hard stools more than 25% of the time
- Incomplete evacuation more than 25% of the time
This might help: Health Screening in Singapore
Symptoms of Constipation
Common symptoms of constipation include:
- Difficulty passing stools
- Passing small, hard, or dry stools
- Feeling bloated or uncomfortable
- Feeling like you haven’t completely emptied your bowels
- Abdominal pain or cramping
- Reduced appetite
- In severe cases, nausea or vomiting
Causes of Constipation

Constipation can be caused by numerous factors, and many patients may have more than one contributing cause. Understanding the underlying cause is crucial for effective treatment.
Lifestyle and Dietary Factors
The most common causes of constipation are related to lifestyle and diet:
- Inadequate fluid intake: Not drinking enough water can make stools hard and difficult to pass
- Low-fiber diet: Insufficient fiber from fruits, vegetables, and whole grains
- Lack of regular exercise: Physical activity helps stimulate intestinal activity
- Ignoring the urge to pass stools: Regularly delaying bowel movements can weaken natural reflexes
- Changes in routine: Travel, changes in diet, or disruptions to daily schedule
- Stress: Excessive or unaccustomed stress can affect digestive function
You might like: Best JB Health Screening Clinics for Singaporeans
Medical Causes
Several medical conditions can cause or contribute to constipation:
- Irritable Bowel Syndrome (IBS): A common digestive disorder affecting the large intestine
- Hypothyroidism: Low thyroid hormone levels can slow down metabolism and digestion
- Neurological conditions: Parkinson’s disease, multiple sclerosis, stroke, spinal cord injuries
- Pregnancy: Hormonal changes and pressure on the intestines from the growing uterus
- Depression and eating disorders: Can affect normal digestive function
- Colorectal cancer: Can cause narrowing of the intestine, leading to constipation
This might help: Irritable Bowel Syndrome (IBS): Causes, Symptoms and Treatment in Singapore
Medication-Related Causes
Various medications can cause constipation as a side effect:
- Calcium or iron supplements
- Antacids containing aluminum or calcium
- Blood pressure medications (especially Nifedipine or Verapamil)
- Strong pain medications (narcotics/opioids)
- Antidepressants
- Antihistamines
Functional Constipation
When no obvious medical cause can be identified, constipation may be classified as functional. This affects up to 30% of patients with constipation and is often under-diagnosed or mismanaged. There are two main types:
- Colonic Inertia: Characterized by poor colon contractions resulting in very infrequent bowel habits (sometimes only 1-2 times per week) and a lack of urge to open bowels
- Obstructed Defecation: A condition where there is usually an urge to pass stools, but the person needs to strain excessively. This may be due to a lack of coordinated anal muscle movements or structural problems like rectal prolapse.
Related article: The Ultimate Guide to Losing Weight in Singapore (2025)
When to See a Doctor
While occasional constipation is common and can often be resolved with self-care measures, you should consult a doctor if you experience any of the following symptoms. These include constipation that is a new and persistent problem lasting more than two weeks, blood or mucus in your stools, or unexplained weight loss.
You should also seek medical attention for severe abdominal pain or cramping, very severe abdominal bloating or wind, and changes in bowel habits, especially when accompanied by weight loss.
Additional warning signs include changes in stool type or texture, loss of appetite, and a history of Inflammatory Bowel Disease (IBD).
Furthermore, constipation alternating with diarrhea, needing to use constipation medication regularly (every 2-3 days or more), and being over 50 with a family history of colorectal cancer are all reasons to consult a healthcare professional.
Related article: Homeopathy in Singapore
Treatment Options for Constipation in Singapore

Self-Care and Lifestyle Modifications
For mild to moderate constipation, these self-care measures are often effective:
1. Increase Fiber Intake
A high-fiber diet can significantly improve bowel regularity and overall digestive health. You should choose brown rice over white rice and wholemeal bread over white bread to increase your fiber consumption.
Fill half your plate with vegetables and include fruits in every meal to ensure adequate fiber intake. Aim for 25-30 grams of fiber daily to maintain healthy bowel function.
Try specific fruits known to help with bowel movements, such as kiwi, prunes, and dragon fruit, which contain natural compounds that promote regularity. However, increase fiber intake gradually to avoid bloating or gas, as sudden increases can cause digestive discomfort.
You might like: Acupuncture in Singapore: Types, Benefits
2. Stay Well-Hydrated
Proper hydration helps keep stools soft and easier to pass. Drink 6-8 glasses (about 2 liters) of fluid daily unless medically advised otherwise by your healthcare provider.
Try different types of drinks, including chrysanthemum tea, barley drinks, herbal teas, milk, and soup to maintain adequate hydration.
Start your day with warm water to stimulate bowel movements and encourage natural digestive processes. Keep a water bottle with you as a reminder to drink regularly throughout the day.
3. Regular Exercise
Physical activity stimulates intestinal muscles and promotes healthy bowel function. Aim for at least 30 minutes of moderate exercise daily to maintain digestive health.
Even light activities like walking can help improve bowel function and overall well-being. Try specific exercises that target abdominal muscles to strengthen the core and support digestive processes.
4. Proper Toileting Habits
Establishing good toileting habits can prevent and relieve constipation effectively. Respond promptly to the urge to defecate rather than delaying or suppressing the natural urge.
Create a regular toileting routine, preferably after meals when the gastrocolic reflex is strongest and most effective. Ensure a comfortable position on the toilet by leaning forward with a straight back, with feet flat or on a footstool so that knees are higher than hips.
Allow sufficient time for bowel movements without rushing, as stress and hurrying can interfere with natural processes. Practice abdominal massage in a clockwise direction to stimulate bowel function and encourage movement.
5. Include Probiotics
Probiotics can help maintain healthy gut flora and support digestive balance. Consume low-sugar or no-sugar-added yogurts that contain live, beneficial bacteria.
Include fermented foods like kimchi, tempeh, and live-culture drinks in your diet to promote a healthy gut microbiome.
Over-the-Counter Medications
If lifestyle changes don’t provide sufficient relief, several over-the-counter remedies are available in Singapore:
1. Bulk-Forming Agents
These medications absorb water and expand in the intestines, creating larger, softer stools that are easier to pass. Ispaghula Husk is a natural fiber supplement that adds bulk to stools and promotes regular bowel movements.
This option is best for mild constipation, especially when related to a low-fiber diet. When using these products, they must be taken with plenty of water, and results may take a few days to become apparent.
2. Osmotic Laxatives
These medications work by drawing water into the intestines to soften stools and increase bowel movements. Lactulose Syrup is a synthetic sugar that is not absorbed by the body but helps retain water in the intestines.
Macrogol powder (Polyethylene glycol) creates softer, easier-to-pass stools by increasing water content. Forlax powder works similarly to Macrogol and provides comparable benefits.
These options are best for moderate constipation, including in elderly patients who may need gentler treatment. Start with a low dose and increase gradually if needed to avoid digestive upset.
3. Stimulant Laxatives
These medications stimulate the intestinal muscles to contract more strongly and promote bowel movements. Bisacodyl Tablets or Suppositories stimulate intestinal muscles directly to encourage movement.
Senna Tablets are plant-based stimulant laxatives that work through natural compounds. These options are best for occasional constipation or when quick relief is needed. Use only short-term, as regular use can lead to dependency and reduced natural bowel function.
4. Stool Softeners
These medications help moisten stools, making them easier to pass without straining. Glycerin Suppositories and Gel lubricate and soften stools for easier elimination.
This option is best for hard, dry stools that are difficult to pass. These products provide relatively quick relief when inserted rectally and are useful for immediate symptom management.
5. Enemas
These treatments introduce fluid directly into the rectum to stimulate bowel movements quickly. Fleet Enema provides rapid relief of constipation through direct rectal administration.
This option is best for severe constipation requiring immediate relief. Use for occasional situations only, not for regular management, as frequent use can disrupt natural bowel function.
Medical Investigations and Treatments
For persistent or severe constipation, medical investigation may be necessary to identify underlying causes:
Diagnostic Tests
Healthcare providers may recommend several diagnostic tests to evaluate constipation causes. Blood tests can check for hormonal imbalances like hypothyroidism that may contribute to digestive issues.
Imaging studies, including CT colonography or barium studies, help exclude growths or structural abnormalities.
Colonoscopy allows direct examination of the colon for issues like colorectal cancer or other pathological conditions.
Transit marker study evaluates how quickly food moves through the digestive system to identify motility problems.
Anorectal manometry tests anal and rectal pressure and muscle coordination to assess function. Defecography uses X-ray or MRI to evaluate actual movements during bowel function and identify mechanical issues.
This might help: Acid Reflux and GERD in Singapore: Causes, Symptoms, and Treatments
Specialized Treatments
For functional constipation that doesn’t respond to conservative measures:
Pelvic Floor Rehabilitation (Anorectal biofeedback) trains anal muscles to contract and relax effectively through guided exercises and feedback. This treatment is particularly helpful for obstructed defecation syndrome where muscle coordination is impaired.
Transanal Irrigation involves a self-administered water enema that clears the bowel at regular intervals. This method is useful for neurogenic bowel dysfunction or severe constipation that doesn’t respond to other treatments.
Neuromodulation (Sacral nerve stimulation) involves inserting a fine electrode near nerves that control bowel function. This advanced treatment can help modulate colonic contractions in colonic inertia where normal muscle function is impaired.
Surgical Options may be considered in extreme cases and include surgical repair of rectal prolapse (rectopexy) for structural problems. In very rare situations, surgical removal of part of the colon may be necessary, though this option is rarely used nowadays due to advances in other treatment methods.
Special Considerations
Constipation During Pregnancy
Pregnancy can significantly increase the risk of constipation due to hormonal changes and physical factors. To manage constipation safely during pregnancy, increase water and fiber intake to promote natural bowel movements.
Gentle exercise like walking or swimming can help stimulate digestive function and overall health during pregnancy. Always discuss safe medications with your doctor before taking any treatments, as many medications may not be suitable during pregnancy.
Never take laxatives without medical advice during pregnancy, as some products may pose risks to both mother and baby.
Constipation in Children
Constipation in children requires special attention and age-appropriate treatment approaches. Treatment often involves disimpaction (clearing out hard stools) followed by maintenance therapy to prevent recurrence.
Diet modifications should include fiber-rich foods appropriate for the child’s age and developmental stage.
Establishing regular toileting habits is crucial for long-term success and preventing chronic constipation issues.
For babies over 2 months, diluted fruit juices like prune juice can help soften stools and promote bowel movements.
For older children, a footstool at the toilet helps create a proper squatting position that facilitates easier bowel movements. Always consult a pediatrician if constipation persists or is severe, as underlying medical conditions may need to be evaluated.
Constipation in the Elderly
Older adults are particularly prone to constipation due to multiple age-related factors that affect digestive function. These factors include decreased mobility, which reduces the natural stimulation of intestinal muscles.
Medication effects from multiple prescriptions can slow bowel function and contribute to constipation. Weakened abdominal muscles also make it more difficult to generate the pressure needed for effective bowel movements.
Treatment should focus on prevention through proper diet, adequate hydration, and appropriate physical activity within the person’s capabilities.
Medication review by a doctor is often helpful to identify and adjust medications that may be contributing to constipation.
Constipation and Hemorrhoids
Chronic constipation can lead to or worsen hemorrhoids (piles), creating a cycle of digestive discomfort.
Excessive straining during constipation can cause hemorrhoids to enlarge and become painful, making bowel movements even more difficult.
Keeping stools soft and regular helps prevent hemorrhoid complications and reduces the need for straining. If constipation continues to irritate hemorrhoids despite conservative treatment, medical intervention may be required to address both conditions.
In severe cases, surgical removal of hemorrhoids (hemorrhoidectomy) may be necessary when conservative treatments fail to provide adequate relief.
Prevention Strategies
Preventing constipation is often easier than treating it, and implementing effective strategies can significantly reduce the likelihood of developing this condition.
Key prevention strategies include maintaining a high-fiber diet with plenty of fruits, vegetables, and whole grains to ensure adequate bulk and nutrition for healthy bowel function.
Staying well-hydrated throughout the day helps keep stools soft and easier to pass. Regular physical activity stimulates intestinal muscles and promotes overall digestive health.
Establishing and maintaining consistent bathroom habits helps train the body’s natural rhythms and promotes regularity. Responding promptly to the urge to defecate prevents stools from becoming harder and more difficult to pass.
Managing stress through relaxation techniques can help maintain healthy digestive function, as stress can significantly impact bowel habits.
Being aware of medications that might cause constipation allows for proactive management and discussion with healthcare providers about alternatives when possible.
Regular health check-ups are important, especially if you have risk factors for constipation, to monitor digestive health and address any developing issues early.
Healthcare Resources in Singapore
Singapore offers excellent healthcare resources for managing constipation:
- Polyclinics: Provide primary care services and can refer to specialists if needed
- Gastroenterologists: Specialists in digestive disorders, available at major hospitals
- Colorectal surgeons: For surgical management of severe cases
- Dietitians: For personalized dietary advice to manage constipation
- Physiotherapists: Can help with pelvic floor rehabilitation
Conclusion
Constipation is a common condition that affects many Singaporeans, but with proper understanding and management, most cases can be effectively treated.
While occasional constipation can usually be resolved with lifestyle modifications and over-the-counter remedies, persistent or severe symptoms warrant medical attention to rule out underlying conditions.
By adopting preventive measures, seeking appropriate treatment, and consulting healthcare professionals when needed, you can effectively manage constipation and maintain good digestive health.
Frequently Asked Questions
How is constipation defined medically?
Constipation is medically defined as having fewer than three bowel movements per week, or having stools that are hard, dry, and difficult to pass, often accompanied by straining.
For diagnostic purposes, doctors often use the Rome IV criteria, which requires two or more of the following symptoms for at least three months: straining during more than 25% of defecations, hard stools more than 25% of the time, incomplete evacuation more than 25% of the time, or a need for manual maneuvers to facilitate defecation.
Can stress cause constipation?
Yes, stress can significantly impact digestive function and contribute to constipation. When stressed, your body enters a “fight or flight” mode, which can slow down digestive processes as blood and energy are diverted to other systems. Stress also affects the gut-brain connection, potentially altering gut motility and leading to irregular bowel movements. Practicing stress-reduction techniques such as meditation, deep breathing exercises, or regular physical activity may help alleviate stress-related constipation.
Are there any natural remedies for constipation?
Several natural remedies may help relieve constipation. These include increasing water intake, consuming high-fiber foods (especially prunes, kiwi, and flaxseeds), regular exercise, and establishing consistent bathroom routines.
Some people find relief with a morning warm water and lemon drink or a tablespoon of olive oil on an empty stomach. Certain herbal teas like senna, dandelion, or peppermint may also stimulate bowel movements.
However, natural remedies should be used appropriately, and persistent constipation warrants medical attention.
How long can a person safely go without a bowel movement?
While normal bowel frequency varies widely among individuals, most healthcare professionals become concerned when a person has not had a bowel movement for more than three days, as stools become harder and more difficult to pass the longer they remain in the colon.
However, if you’re not experiencing discomfort, bloating, or pain, going a few days without a bowel movement may be normal for your body. If constipation lasts more than a week or is accompanied by severe symptoms, medical attention should be sought.
Can certain foods cause constipation?
Yes, certain foods can contribute to constipation. Foods low in fiber and high in fat or refined carbohydrates often slow down digestion. Common culprits include processed foods, dairy products (especially cheese), white bread and rice, unripe bananas, red meat, fried foods, and foods high in sugar.
Additionally, some people may experience constipation after consuming eggs or chocolate. Individual responses to these foods vary, so it’s helpful to keep a food diary if you suspect dietary triggers for your constipation.
Is it safe to use laxatives regularly?
Regular use of laxatives, especially stimulant laxatives, is generally not recommended as it can lead to dependency. The body may begin to rely on laxatives for bowel movements, potentially weakening natural bowel function over time.
Bulk-forming laxatives (fiber supplements) are generally the safest for longer-term use, followed by osmotic laxatives. If you find yourself needing laxatives regularly (more than 2-3 times per week for several weeks), it’s important to consult a healthcare provider to address the underlying cause of your constipation.
How does exercise help with constipation?
Exercise helps with constipation in several ways. Physical activity stimulates the muscles in the intestines, promoting peristalsis (the wave-like contractions that move food through the digestive tract).
This increased muscle activity helps move stool through the colon more efficiently. Exercise also reduces the time food takes to move through the large intestine, limiting the amount of water absorbed from the stool and helping prevent hard, dry stools.
Additionally, regular physical activity helps reduce stress, which can be a contributing factor to constipation.
What is the relationship between constipation and hemorrhoids?
Constipation and hemorrhoids have a strong cause-and-effect relationship. When constipated, people often strain during bowel movements to pass hard, dry stools.
This straining increases pressure in the rectal and anal veins, which can cause these blood vessels to swell and form hemorrhoids.
The passage of hard stools can also irritate existing hemorrhoids, causing pain, bleeding, and further swelling.
Preventing constipation through proper diet, hydration, and bowel habits is one of the most effective ways to prevent hemorrhoids or prevent existing hemorrhoids from worsening.
Can constipation cause back pain?
Yes, severe constipation can sometimes cause back pain. When stool builds up in the colon, it can create pressure and discomfort that radiates to the lower back.
This is particularly common when constipation leads to impaction (a large, hard mass of stool that becomes stuck in the rectum or colon).
The backup of stool can also cause the colon to expand, putting pressure on surrounding structures and nerves in the back.
If you’re experiencing back pain along with constipation, it’s important to address the constipation and consult a healthcare provider if symptoms persist.
What dietary changes are most effective for preventing constipation?
The most effective dietary changes for preventing constipation include increasing fiber intake gradually to 25-30 grams daily through whole grains, fruits, vegetables, legumes, and nuts; staying well-hydrated by drinking at least 8 glasses of water daily; incorporating probiotic-rich foods like yogurt and fermented vegetables; consuming natural laxative foods such as prunes, kiwi, and flaxseeds; reducing processed foods, cheese, and refined carbohydrates; and limiting alcohol and caffeine, which can contribute to dehydration.
Establishing regular mealtimes may also help regulate bowel movements, as the gastrocolic reflex (the body’s natural urge to defecate after eating) is strongest after meals, particularly breakfast.
How does aging affect bowel function and constipation risk?
Aging increases the risk of constipation due to several factors. Older adults often experience decreased muscle tone in the digestive tract, leading to slower movement of food through the colon.
Many seniors take multiple medications that may have constipation as a side effect. Reduced mobility and physical activity, common in older populations, can slow bowel function. Seniors may also consume less fiber and fluids due to decreased appetite or dental issues.
Additionally, neurological changes related to aging can affect the nerves controlling bowel function. Managing constipation in older adults often requires a multifaceted approach addressing medication review, diet, hydration, and appropriate physical activity.
What’s the difference between chronic and acute constipation?
Acute constipation is a sudden onset of difficult or infrequent bowel movements that typically lasts for a short period (days to weeks) and often has an identifiable cause such as dietary changes, travel, medication, or illness.
It usually resolves when the underlying issue is addressed. Chronic constipation, by contrast, persists for at least three months and involves ongoing symptoms like straining, hard stools, or incomplete evacuation.
Chronic constipation may be functional (no identifiable organic cause) or secondary to underlying conditions. Treatment approaches differ, with acute constipation often responding to simple interventions while chronic constipation may require comprehensive evaluation and long-term management strategies.
Can probiotics help with constipation?
Research suggests that certain probiotic strains may help alleviate constipation by improving gut transit time, stool consistency, and bowel movement frequency. Probiotics can help restore a healthy balance of gut bacteria, which plays a crucial role in digestion and bowel function.
Strains that have shown benefit for constipation include Bifidobacterium lactis, Lactobacillus casei Shirota, and Bifidobacterium longum. Probiotic foods include yogurt with live cultures, kefir, kimchi, sauerkraut, and tempeh.
hile probiotics show promise as a complementary approach, they work best when combined with other constipation management strategies like adequate fiber, hydration, and physical activity.

