What is Deep Vein Thrombosis?
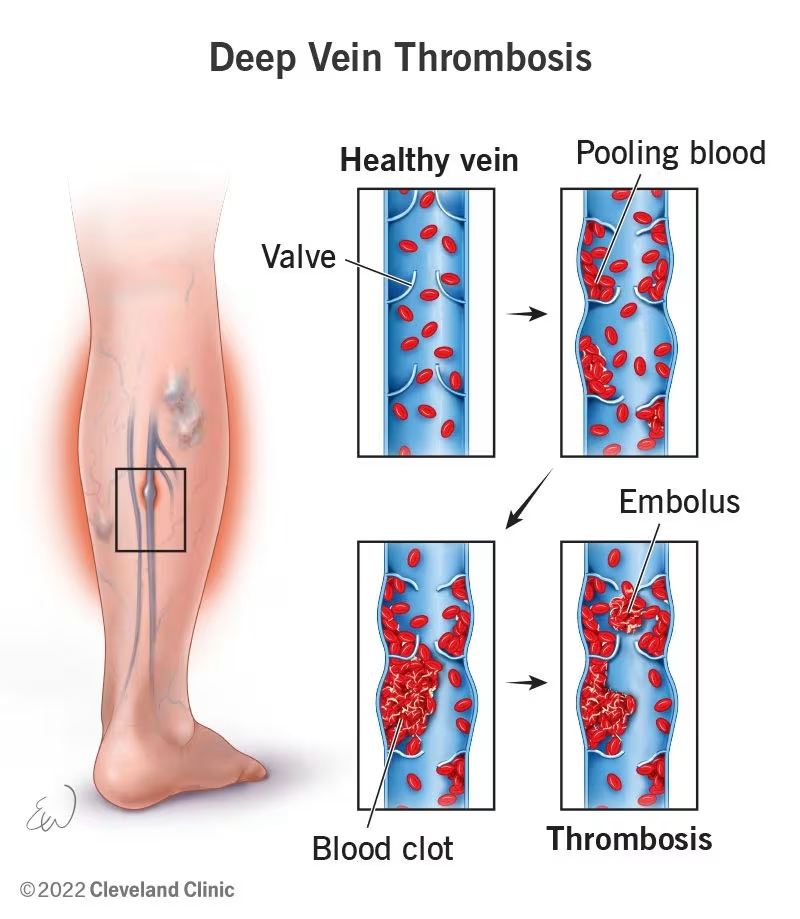
Deep vein thrombosis (DVT) is a serious medical condition characterized by the formation of a blood clot (thrombus) in a vein located deep within the body.
While these clots most commonly develop in the lower extremities—specifically in the leg or thigh veins—they can also occur in other areas such as the arms, intestines, liver, or kidneys.
The danger of DVT lies in its potential complications. The blood clot may interfere with normal circulation and, more alarmingly, could break off and travel through the bloodstream to the lungs.
When a clot lodges in the pulmonary arteries, it causes a potentially life-threatening condition called pulmonary embolism (PE).
Together, DVT and PE are collectively referred to as venous thromboembolism (VTE), sharing the same risk factors and often requiring similar preventive measures.
You might be interested: Health Screening in Singapore
Symptoms of Deep Vein Thrombosis
An important characteristic of DVT is that approximately half of those affected may not experience any symptoms, particularly in less severe cases. However, when symptoms do appear, they typically include:
- Swelling in the affected limb, usually starting in the calf and potentially extending upward
- Pain or tenderness in the leg, often described as a cramping sensation that may worsen when standing or walking
- Increased warmth in the swollen or painful area
- Skin discoloration—the affected area may appear red, pale, or bluish
- Prominent veins visible under the skin
If DVT occurs in the arms, which is less common, typical symptoms include:
- Neck pain
- Shoulder pain
- Swelling in the forearms that may extend toward the heart
- Weakness in the affected arm
The absence of symptoms doesn’t mean the condition is less dangerous. Even asymptomatic DVT can lead to serious complications if not detected and treated appropriately.
You might like: Best JB Health Screening Clinics for Singaporeans
Pulmonary Embolism: A Life-Threatening Complication
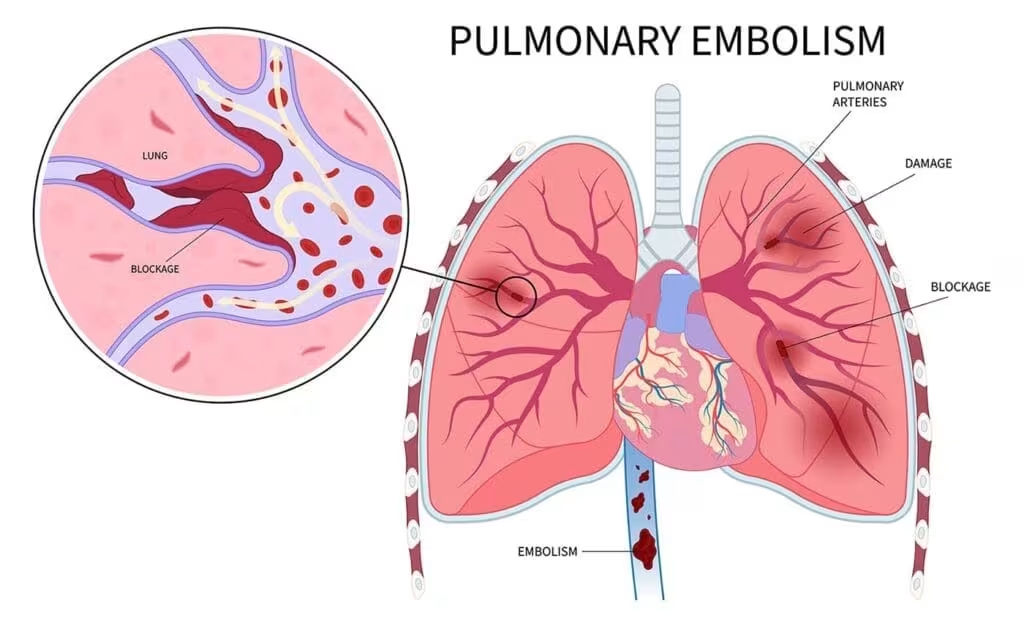
The most concerning complication of DVT is pulmonary embolism (PE), which occurs when a fragment of the blood clot breaks away, travels through the bloodstream, and becomes lodged in the lungs.
This medical emergency requires immediate attention and can be fatal if not treated promptly.
Symptoms of pulmonary embolism include:
- Chest pain, especially when taking a deep breath
- Rapid pulse
- Sudden shortness of breath
- Fainting or feeling lightheaded
- Coughing up blood
If you experience these symptoms, especially after having DVT symptoms or risk factors, seek emergency medical care immediately.
Read more: Comprehensive Guide to Coronary Angioplasty in Singapore
Risk Factors for Deep Vein Thrombosis
Multiple factors can increase your likelihood of developing DVT. Understanding these risk factors is crucial for prevention, especially if you have several of them:
Immobility and Inactivity
Prolonged bed rest poses a significant risk, particularly for individuals with paralysis or those requiring extended hospitalization.
Long periods of sitting, such as during long-haul flights or extended car journeys, can also contribute to clot formation.
When the legs remain immobile for extended periods, the muscles don’t contract properly, which reduces blood circulation and increases the risk of clotting.
Surgery and Injury
Surgical procedures carry increased risk, especially those involving the legs, pelvis, or abdomen. Major trauma or injuries that damage blood vessel walls can also trigger clot formation.
Both surgical procedures and traumatic injuries can stimulate clot formation as part of the body’s natural healing response.
This might help: Which Cardiologist in Singapore Should You Consider? (Sort by Reviews)
Medical Conditions
Several medical conditions increase DVT risk, including cancer and certain cancer treatments. Heart and lung diseases, inflammatory bowel disease, and nephrotic syndrome (a kidney condition) all contribute to elevated risk.
Additionally, hypercoagulable states—conditions that increase the blood’s natural tendency to clot—significantly raise the likelihood of developing DVT.
Hormonal Influences
Pregnancy and the postpartum period create hormonal changes that increase clotting risk. Oral contraceptive use and hormone replacement therapy also elevate risk factors.
These conditions increase estrogen levels, which can boost blood clotting proteins in the body.
Personal Factors
Age over 60 increases DVT risk, although the condition can occur at any age. Obesity, smoking, and a personal or family history of DVT are significant risk factors.
Severe varicose veins also contribute to increased clotting risk.
Anatomical Variations
Certain anatomical conditions can predispose individuals to DVT, including May-Thurner Syndrome and Paget-Schroetter Syndrome.
These conditions disrupt normal blood flow patterns and significantly increase clotting risk.
Related article: The Ultimate Guide to Losing Weight in Singapore
Diagnosis of Deep Vein Thrombosis
When DVT is suspected, prompt and accurate diagnosis is essential. Your healthcare provider will:
- Evaluate your medical history and symptoms to assess your risk factors and clinical presentation
- Perform a physical examination to check for signs such as swelling, tenderness, and skin changes
- Order diagnostic tests, which may include:
- Duplex Ultrasound: The primary diagnostic tool for DVT, this non-invasive test visualizes blood flow through the veins and can detect abnormalities indicative of clotting
- D-dimer blood test: Elevated levels indicate increased clotting activity in the body
- CT scan or MRI: May be used in complex cases or to examine veins in areas difficult to assess with ultrasound
- Venography: A specialized X-ray procedure using contrast dye, typically reserved for cases where other tests are inconclusive
Early diagnosis allows for prompt treatment, reducing the risk of complications and improving outcomes.
Treatment Options for Deep Vein Thrombosis
The primary goal of DVT treatment is to prevent the clot from growing larger, reduce the risk of new clots forming, and minimize the likelihood of pulmonary embolism. Treatment strategies include:
Anticoagulation Therapy (Blood Thinners)
The cornerstone of DVT treatment involves medications that inhibit the blood’s clotting ability:
- Injectable anticoagulants:
- Heparin
- Low molecular weight heparin (LMWH)
- Often used initially for rapid effect
- Oral anticoagulants:
- Warfarin (requires regular monitoring)
- Direct oral anticoagulants (DOACs) like apixaban, dabigatran, and rivaroxaban (generally require less monitoring)
The duration of anticoagulation therapy varies depending on your specific circumstances, ranging from three months to indefinite treatment for recurrent DVT.
Minimally Invasive Procedures
For severe or extensive DVT that doesn’t respond adequately to anticoagulation alone, interventional procedures may be considered:
- Thrombolysis: A catheter-based technique that delivers clot-dissolving medications directly to the affected vein
- Thrombectomy: Mechanical removal of the clot using specialized devices
- Vena cava filter placement: A filter inserted into the large vein that returns blood from the lower body to the heart, designed to trap clots before they can reach the lungs
These procedures are typically performed through small incisions, allowing for efficient clot removal with minimal invasiveness. They’re often reserved for cases where:
- The DVT is extensive
- There’s a high risk of pulmonary embolism
- Anticoagulation therapy is contraindicated
- The patient has developed pulmonary embolism despite anticoagulation
Compression Therapy

- Prescription-strength compression stockings apply graduated pressure to improve blood flow
- Help reduce swelling and pain
- May prevent post-thrombotic syndrome, a long-term complication of DVT
Prevention of Deep Vein Thrombosis
Preventing DVT is particularly important for those with multiple risk factors. Effective preventive strategies include:
Lifestyle Modifications
- Regular physical activity: Exercise promotes healthy blood circulation
- Maintaining a healthy weight: Obesity increases DVT risk
- Quitting smoking: Smoking negatively affects blood circulation
- Staying hydrated: Adequate fluid intake prevents blood from thickening
- Avoiding prolonged immobility: Change positions frequently during long periods of sitting
This might help: Acid Reflux and GERD in Singapore: Causes, Symptoms, and Treatments
During Long-Distance Travel
- Keep moving: Don’t remain in a cramped position for extended periods
- Wiggle your toes and flex your ankles regularly
- Stand up and walk around when possible (at least every 1-2 hours)
- Request an aisle seat on flights for easier movement
- Practice proper posture: Avoid crossing your legs or sitting on the edge of your seat
- Wear appropriate clothing: Choose loose-fitting attire and avoid restrictive socks or stockings
- Stay hydrated: Drink water regularly while avoiding alcohol and caffeine, which can contribute to dehydration
- Consider compression stockings: Travel-specific compression socks can promote venous blood flow in the lower limbs
- Avoid sleeping pills during flights: These encourage immobility and increase DVT risk
Medical Prevention for High-Risk Situations
If you’re undergoing surgery or have multiple risk factors, your doctor may recommend:
- Prophylactic anticoagulants: Low-dose blood thinners to prevent clot formation
- Intermittent pneumatic compression devices: These inflate and deflate around the legs to promote blood flow
- Graduated compression stockings: Specialized stockings that apply varying pressure to improve circulation
Long-Term Complications of DVT
Post-Thrombotic Syndrome (PTS)
This chronic condition develops in 20-50% of DVT patients and occurs when the affected vein is damaged by the clot, leading to:
- Chronic pain and swelling
- Skin discoloration
- Venous ulcers in severe cases
- Impaired mobility and quality of life
Wearing prescribed compression stockings for at least two years following DVT can significantly reduce the risk of developing PTS.
This might help: Celiac Disease Treatment in Singapore
Recurrent DVT
Having one episode of DVT increases your risk of experiencing another. Adhering to your treatment plan and implementing preventive measures is crucial for minimizing this risk.
When to Seek Medical Attention
Prompt medical evaluation is essential if you experience symptoms of DVT or pulmonary embolism, have multiple risk factors for DVT, or notice worsening of existing DVT symptoms.
For those on anticoagulant therapy, seek immediate medical attention if you develop prolonged or excessive bleeding, blood in urine or stool, bleeding gums, or extended nosebleeds.
Additionally, contact your healthcare provider immediately if you experience coughing up blood, unusual weakness, dizziness, headaches, or unexplained swelling.
Managing DVT in Daily Life
If you’ve been diagnosed with DVT, following specific recommendations for daily management is crucial for your health and recovery.
Take medications exactly as prescribed and never skip doses of anticoagulants, as consistent medication adherence is vital for treatment success.
Attend all follow-up appointments to ensure regular monitoring and effective treatment.
Wear compression stockings as directed by your healthcare provider and stay active by resuming physical activity gradually as advised by your doctor.
Always consult your doctor before taking new medications, since some drugs can interact with anticoagulants.
Maintain a balanced diet that focuses on fruits, vegetables, and whole grains while limiting alcohol consumption, as alcohol can interfere with anticoagulant medications.
Avoid high-risk activities by discussing with your doctor which activities might increase bleeding risk.
Finally, carry medical identification to inform others of your condition in case of emergency.
DVT Care in Singapore
Singapore offers comprehensive care for DVT patients through several specialized services and facilities.
The healthcare system provides advanced diagnostic facilities with state-of-the-art imaging technology and access to specialized vascular surgeons and interventional radiologists.
Well-established anticoagulation monitoring services ensure proper medication management, while a multidisciplinary approach to DVT management provides comprehensive patient care.
Whether you’re experiencing symptoms, have risk factors, or need ongoing care for diagnosed DVT, Singapore’s healthcare system provides access to high-quality medical expertise for this potentially serious condition.
FAQs
What’s the difference between DVT and superficial vein thrombosis?
Deep vein thrombosis occurs in veins situated deep within the body, particularly those near bones and deep muscles that carry the majority of blood from the limbs to the heart. In contrast, superficial vein thrombosis affects veins just beneath the skin. While both involve blood clots, DVT is generally more serious with greater risk of complications like pulmonary embolism.
How long does DVT treatment typically last?
The duration of DVT treatment varies based on individual factors. Most patients require anticoagulation therapy for at least three months.
However, treatment may extend to six months or longer for unprovoked DVT or indefinitely for those with recurrent DVT or ongoing risk factors. Your doctor will determine the appropriate treatment duration based on your specific situation.
Can I exercise with DVT?
Initially after DVT diagnosis, strenuous exercise should be avoided while the clot stabilizes. However, gentle movement is typically encouraged to promote circulation.
As treatment progresses, physical activity can gradually increase under medical guidance. Walking is often recommended, while activities with high impact or injury risk may be restricted.
Always consult your healthcare provider about an appropriate exercise plan for your specific condition.
Will I need to take blood thinners forever after having DVT?
Not necessarily. The duration of anticoagulant therapy depends on several factors, including whether your DVT was provoked by a temporary risk factor (like surgery) or unprovoked, whether you’ve had previous clots, and your overall risk profile. Some patients require only 3-6 months of treatment, while others with recurrent DVT or certain clotting disorders may need lifelong therapy.
Your doctor will evaluate your individual situation to determine the appropriate duration.
Does flying increase my risk of DVT?
Yes, long-haul flights (typically over 4 hours) can increase DVT risk due to prolonged immobility in confined spaces. This risk is higher for those with additional risk factors such as previous DVT, pregnancy, recent surgery, cancer, or genetic clotting disorders.
Studies indicate that passengers in window seats have approximately double the risk compared to those in aisle seats due to reduced mobility.
Preventive measures include regular movement, staying hydrated, wearing compression stockings, and avoiding alcohol and sleeping pills during flights.
How is DVT diagnosed during pregnancy?
Diagnosing DVT during pregnancy involves special considerations. While clinical evaluation remains important, D-dimer blood tests are less useful as they naturally increase during pregnancy.
Doppler ultrasound is the preferred diagnostic method as it avoids radiation exposure. If additional imaging is needed, MRI may be used instead of CT scans to avoid radiation.
Pregnant women with suspected DVT should be evaluated promptly, as pregnancy increases clotting risk by 4-5 times compared to non-pregnant women.
What is May-Thurner Syndrome and how does it relate to DVT?
May-Thurner Syndrome is an anatomical condition where the right iliac artery compresses the left iliac vein in the pelvis, restricting blood flow and increasing DVT risk in the left leg.
This compression creates turbulence in blood flow and potential vessel wall damage, creating favorable conditions for clot formation.
People with May-Thurner Syndrome have a significantly higher risk of developing left-sided DVT. Treatment may involve stent placement to keep the vein open, alongside conventional DVT management with anticoagulation.
Can children develop DVT?
Yes, although DVT is much less common in children than adults. When it occurs in children, it’s often associated with underlying risk factors such as central venous catheters, cancer, congenital heart disease, trauma, surgery, or inherited clotting disorders.
Symptoms mirror those in adults but may be more difficult to identify. Diagnosis and treatment principles are similar, though medication dosing differs. Children with DVT require care from specialists experienced in pediatric thrombosis management.
What dietary considerations should I keep in mind while on anticoagulants?
If you’re taking warfarin, maintain consistent vitamin K intake as dramatic changes can affect the medication’s effectiveness.
Foods high in vitamin K include green leafy vegetables, broccoli, and Brussels sprouts. For those on direct oral anticoagulants (DOACs) like apixaban or rivaroxaban, dietary restrictions are fewer, but certain foods and supplements (like cranberry products, grapefruit, St. John’s Wort) may still interact with these medications.
Limit alcohol consumption and stay well-hydrated regardless of which anticoagulant you’re prescribed. Always discuss specific dietary guidelines with your healthcare provider.
How soon can I return to work after DVT diagnosis?
The timeline for returning to work depends on multiple factors including the severity of your DVT, your treatment response, and the physical demands of your job.
Desk-based roles with limited physical activity may allow a return within days or 1-2 weeks, while jobs requiring significant physical exertion might necessitate several weeks of recovery.
Your doctor will provide personalized guidance based on your specific situation. Gradual reintegration with modified duties is often recommended, along with measures to prevent prolonged immobility during work hours.

