Understanding Colorectal Cancer

Colorectal cancer is cancer of the colon (large intestine) and the rectum (the passageway connecting the colon to the anus). It’s Singapore’s top cancer killer, affecting more than 1,865 cases each year.
The disease typically begins as non-cancerous polyps (growths of tissue) on the inner lining of the colon or rectum which may develop into cancer over time.
Most colorectal cancers develop slowly over several years. Before cancer forms, a growth of tissue or tumor usually begins as a non-cancerous polyp on the inner lining of the colon or rectum. Not all polyps change into cancer, and this largely depends on the type of polyp.
The colon is responsible for absorbing water and salts from the food we eat and turns indigestible food into waste. The rectum stores food waste of the body before it is expelled.
Colorectal cancer occurs when cells of the colon or rectum develop genetic mutations that cause cells to grow uncontrollably and form malignant tumors.
Cancer cells from the inner lining can grow deep into the wall of the colon or rectum and may extend into the surrounding fatty tissue and organs. Colorectal cancer can also spread to nearby lymph nodes. In some cases, cancer cells spread through blood vessels to other parts of the body such as the liver and lungs.
Read more: Comprehensive Guide to Colonoscopy in Singapore
Prevalence in Singapore
Colorectal cancer is the second most common cancer in Singapore, affecting 36 out of 100,000 people.
It is the second most common type of cancer for men and women after prostate cancer and breast cancer, respectively. Between 2018-2022, 12,704 cases of colorectal cancer were diagnosed in Singapore.
While colorectal cancer is commonly diagnosed in people aged 50 years and above, there has been a rising incidence amongst younger individuals under the age of 50 globally. Younger individuals who are diagnosed with colorectal cancer may have hereditary conditions including familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (Lynch Syndrome).
Commonly, younger onset colorectal cancers may also be sporadic (non-hereditary) with multiple environmental and lifestyle factors contributing to its development.
Among the races in Singapore, the Chinese have a higher risk of colorectal cancer.
You may be interested: The Ultimate Guide to Losing Weight in Singapore
Risk Factors
You have a higher chance of developing colorectal cancer if you:
- Are over 50 years of age
- Have a family history of colon or rectum cancer
- Have a previous history of colon polyps
- Have a history of ulcerative colitis (ulcers in the lining of the large intestine) or Crohn’s disease
- Have inflammatory bowel diseases that cause inflammation of the intestines
- Have diabetes or insulin resistance
- Have a family history of certain inherited conditions such as Lynch syndrome or familial adenomatous polyposis
- Follow a low-fiber, high-fat diet (a typical Western diet)
- Lead a sedentary lifestyle
- Smoke or consume excessive alcohol
- Are obese
Despite knowledge of these risk factors, the exact cause of colorectal cancer is unknown. It is estimated that 50 percent of colorectal cancer patients have no known risk factors.
You might like: Homeopathy in Singapore
Signs and Symptoms
Colorectal cancer is often a silent disease, developing with no symptoms at all in early stages. When symptoms do occur, they may include:
- A change in bowel habits, including diarrhea or constipation
- Rectal bleeding or blood (either bright red or very dark) in the stool
- Persistent abdominal discomfort such as cramps, gas, or pain
- A feeling that the bowel does not completely empty after opening the bowels
- Incomplete emptying of the bowel
- Unexplained weight loss
- Constant tiredness
- Severe appetite loss
The symptoms above can be caused by a number of reasons and may not indicate the presence of cancer. However, make an appointment with your doctor if you have any signs or symptoms that worry you.
Screening Methods
Regular screening is the best way to detect colorectal polyps or cancer early. In Singapore, the recommended age of screening for colorectal cancer is 50 years old for individuals with no symptoms. Individuals with a family history of colorectal cancer are advised to start screening earlier. Speak with your healthcare provider who will be able to do a risk assessment and advise you on screening recommendations.
Read more: Health Screening in Singapore
Faecal Immunochemical Test (FIT)

The FIT test checks for hidden blood in the stool, which can be an early sign of colorectal cancer. The test comes in a simple kit and can easily be carried out in the comfort of your own home.
You will be given two FIT kits because two stool samples should be collected over two days for a more accurate result.
Screening with FIT should be done once a year. However, if you develop any colorectal cancer symptoms such as blood in stools or changes in bowel habits, please see your doctor immediately even if you had a normal FIT result.
This might help: Best JB Health Screening Clinics for Singaporeans
Colonoscopy
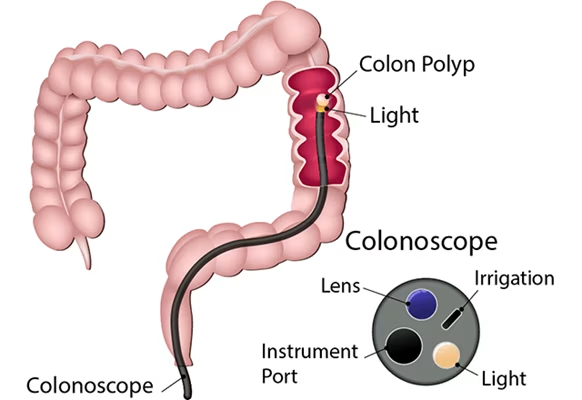
A colonoscopy is a procedure that enables your doctor to examine the lining of your colon for abnormal growths. A soft and flexible tube, about the thickness of a finger, is gently inserted into the anus and advanced into the colon.
The tube has a built-in camera that allows your doctor to see your colon. The procedure usually takes about 15 to 30 minutes to complete.
For screening the general population at average risk, colonoscopy should be performed at an interval of no more than 5 to 10 years.
Other Screening Tests
Other tests that can be used to detect polyps, cancer, or other abnormalities in the colon and rectum include:
- Digital rectal examination
- Flexible sigmoidoscopy
- Computed Tomographic Colonography (CTC)
- Barium enema
You might be interested: Diabetes Myths Debunked: Separating Fact from Fiction
Screening Recommendations by Risk Group
The frequency of screening depends on your risk level. Here’s a table outlining the screening recommendations:
| Risk Group | Onset (Age) | Frequency of colonoscopy screening |
|---|---|---|
| Average Risk | ||
| Asymptomatic or family history limited to non-first degree relatives | 50 years | Every 5 to 10 years |
| Increased Risk | ||
| Colorectal cancer in first degree relative (parent, sibling) age 60 yrs or younger or two or more first degree relatives | 10 yrs prior to youngest case in the family or age 40 yrs, whichever is earlier | Every 5 years |
| Colorectal cancer in first degree relative over the age of 60 yrs | 50 years | Every 5 to 10 years |
| Personal history of colorectal polyps | 1 to 3 yrs after polypectomy in the presence of high risk features (>1cm, multiple, villous architecture); otherwise, 3 to 5 yrs after polypectomy for low risk polyps | – |
| Personal history of colorectal malignancy | One year after resection | Every 1 to 3 years |
| Personal history of ovarian or endometrial cancer | After resection | – |
| High Risk | ||
| Family history of familial adenomatous polyposis | 10 to 12 years (from puberty) | Annually* |
| Family history of hereditary non-polyposis colorectal cancer (Lynch Syndrome) | 20 to 25 yrs | Every 1 to 2 years |
| Inflammatory Bowel Disease | ||
| Left-sided colitis | From 15th yr of diagnosis | Every 1 to 2 years |
| Pan-colitis | From 8th yr of diagnosis | Every 1 to 2 years |
*Flexible sigmoidoscopy from age 10 to 12 years (puberty) until adenomas are identified, upon which screening is switched to colonoscopy
Diagnosis
There are several different tests that can be used to detect polyps, cancer or other abnormalities in the colon and rectum.
Before administering some of these tests, the colon must be emptied, and the doctor may prescribe an enema or a liquid laxative. This preparation is very important in ensuring the test accuracy.
Diagnostic tests include:
- Physical Exam: Your doctor checks general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual.
- Digital Rectal Exam: The doctor inserts a lubricated gloved finger into the rectum to feel for lumps or anything that seems unusual. However, this detects cancer only in the last 5 to 8 centimeters of the rectum.
- Colonoscopy: In addition to diagnosing colorectal cancer, it can also be used to check the entire length of the colorectum for other traces of cancer or the presence of polyps. At the same time, cancer that has been detected can be biopsied or polyps removed.
- CT Scan: This detailed computerized X-ray scan is especially useful for determining the actual extent and location of a cancerous tumor, the invasion of adjacent organs or bowels, and the presence of liver metastases.
- Tumor Markers: The tumor marker for colorectal cancer is carcino-embryonic antigen (CEA). Patients with colorectal cancer may have a high level of CEA. These cancer-specific substances are found in the blood and are useful in monitoring patients for the recurrence of cancer after surgery.
- Biopsy: A diagnosis of cancer is based on a biopsy of polyps or tumors. A tissue sample of the tumor is removed and sent for laboratory analysis.
You might like: Gestational Diabetes Treatment in Singapore
Staging
If diagnosed with colorectal cancer, the doctor may recommend further tests to determine the extent or stage of cancer.
These are usually imaging tests for the abdominal, pelvic, and chest areas.
- Stage 0 (Carcinoma in situ): When there are abnormal or precancerous cells found in the mucosa, or innermost lining of the colon or rectum.
- Stage 1 Colorectal Cancer: When cancer has spread into the deeper layers of the intestinal wall but does not extend beyond the muscle layer.
- Stage 2 Colorectal Cancer: When cancer has penetrated deeper through or beyond the muscle layer of the intestine wall but has not spread to nearby lymph nodes.
- Stage 3 Colorectal Cancer: When cancer has spread to the surrounding regional lymph nodes.
- Stage 4 Colorectal Cancer: When cancer has spread or metastasized to areas beyond the colon or rectum and other organs such as the liver, lungs, and peritoneum.
Treatment Options
Treatment for colorectal cancer depends on the stage, location, size, and histopathological features such as the grade of the cancer.
An individual with colorectal cancer should be assessed by a multi-disciplinary team of specialists to determine which modality of treatment is best suited for them.
Surgery
Surgery is the most common kind of treatment for all stages of colorectal cancer. Depending on the stage of cancer, there are different approaches that the surgeon may use during surgery:
- Local excision: If the cancer is found at a very early stage, the doctor may remove it with colonoscopy (without the need to cut through the abdominal wall). A tube will be put through the rectum into the colon to remove the cancer.
- Resection: If the cancer is larger, the doctor will remove the part of the colon containing the cancer and lymph nodes, along with a small amount of healthy colon on either side of the cancer. This is called colectomy. The ends of the colon are then reconnected. This is called anastomosis. If the doctor is not able to reconnect the two ends of the colon, a stoma is made on the outside of the body for waste to pass through. A bag is placed around the stoma to collect the waste.
Today, many surgeries can be performed using minimally invasive surgical techniques (key-hole surgery). Minimally invasive surgery has been shown to result in faster recovery with less postoperative pain.
Radiation Therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
Radiation therapy is usually used after surgical removal of the cancer to destroy any residual cancer cells within the site of the cancer. It can also be used together with chemotherapy to shrink a large colorectal cancer before surgery.
Radiation therapy is administered in daily sessions, 5 days per week over 4 to 6 weeks.
Side effects are usually tolerable and temporary and range from abdominal cramps and pain, constipation or diarrhea, cystitis, excoriation of perianal skin, and generalized tiredness.
Chemotherapy
Chemotherapy is the use of drugs to stop the growth of cancer. It can be administered by injecting drugs into the vein or taken by mouth as pills.
Depending on the stage of the cancer, chemotherapy may be required after surgery to prevent recurrence and improve a person’s chance of survival.
Chemotherapy is commonly used for patients with advanced colorectal cancer which cannot be cured by surgery or have spread to other parts of the body.
The many different treatment options available have enabled advanced colorectal cancer patients to live longer despite having an incurable cancer and they are managed with having a chronic condition.
Targeted Therapy and Immunotherapy
Treatment for advanced colorectal cancer is now personalized whereby genetic information from the cancer is used to guide the selection of medications such as targeted therapy and immunotherapy.
- Targeted therapy uses drugs to help stop cancer from growing and spreading. They work by targeting specific genes or proteins found in cancer cells or in cells related to cancer growth, like blood vessel cells.
- Immunotherapy is a treatment that uses the patient’s own immune system to fight cancer. It is given intravenously and is usually used in selected cases of patients with microsatellite instability high (MSI-H) or deficient mismatch repair (dMMR) colorectal cancers. MSI-H/dMMR colorectal cancer may be linked to a hereditary type of colorectal cancer syndrome called Lynch Syndrome or may be sporadic (non-hereditary).
Supportive (Palliative) Care
Palliative care is specialized medical care that provides relief from pain and symptoms of serious illness so that a person with cancer feels better and has a better quality of life.
The palliative care team of doctors, nurses, and other healthcare professionals provide an additional layer of support that complements ongoing care.
Prevention of Colorectal Cancer
Regular screening is crucial for early detection and prevention of colorectal cancer. Apart from regular screening, here are some lifestyle changes that can help reduce your risk:
- Healthy Diet: Eat a diet rich in fruits, vegetables, and whole grains which contain fiber and antioxidants. Limit fat intake especially saturated fat from animal sources such as fatty meat, red meat, and full cream dairy products.
- Regular Exercise: Maintain a healthy weight and stay physically active. Physical activity improves the movement of feces in the colon and can reduce risk.
- Limit Alcohol: Restrict alcohol consumption as drinking copious amounts of alcohol can increase the risk of colorectal cancer.
- Quit Smoking: As with most cancers, smoking is a risk factor for developing colorectal cancer.
- Regular Screening: Follow the recommended screening guidelines based on your risk factors.
FAQ
What is the most common age for developing colorectal cancer?
Colorectal cancer is commonly diagnosed in people aged 50 years and above. However, there has been a rising incidence amongst younger individuals under the age of 50 globally.
How often should I get screened for colorectal cancer?
For average-risk individuals, screening for colorectal cancer should begin at age 50 years. FIT is one of the recommended screening tests and should be performed annually.
Colonoscopy is recommended every 5 to 10 years. If you have increased risk factors, you may need to start screening earlier and more frequently.
Is colorectal cancer hereditary?
Some cases of colorectal cancer are hereditary, particularly those associated with genetic syndromes like Lynch syndrome or familial adenomatous polyposis (FAP). Family history is an important factor in assessing risk.
What is the survival rate for colorectal cancer?
The survival rate depends on the stage of the cancer when it’s diagnosed. Colorectal cancer can be cured when it is diagnosed and treated when localized (stage I-III).
With medical advancements, treatment may also be potentially curative for a smaller subset of patients with stage IV colorectal cancer that has limited spread amenable to surgery or ablation.
Can colorectal cancer be prevented?
While not all colorectal cancers can be prevented, regular screening can often detect colorectal cancer early, when it is most likely to be curable.
In many cases, screening can also prevent colorectal cancer as some polyps or growths can be removed before they have the chance to develop into cancer.
What is the difference between colon cancer and rectal cancer?
Colon cancer and rectal cancer refer to cancer that begins in the large intestine (colon) or the rectum (end of the colon), respectively.
While they are often referred to together as colorectal cancer because they share many features, their treatment might differ especially in the use of radiation therapy and the surgical approach.
What are the symptoms of advanced colorectal cancer?
Advanced colorectal cancer may cause symptoms such as persistent abdominal pain, unexplained weight loss, weakness and fatigue, nausea and vomiting, jaundice (if the cancer has spread to the liver), and difficulty breathing (if the cancer has spread to the lungs).
How is the FIT test different from a colonoscopy?
The FIT test checks for hidden blood in the stool, which can be an early sign of colorectal cancer. It is a non-invasive screening method that can be done at home.
Colonoscopy, on the other hand, is a procedure that allows direct visualization of the colon and rectum, and enables the doctor to remove any polyps found during the procedure.
While the FIT test should be done annually, a colonoscopy is typically recommended every 5 to 10 years for average-risk individuals.
Are there any dietary recommendations for colorectal cancer prevention?
A diet rich in fruits, vegetables, and whole grains may help reduce the risk of colorectal cancer. It’s also advisable to limit the consumption of red meat and processed meats.
Maintaining a healthy weight and regular physical activity are also important factors in colorectal cancer prevention.
What should I expect during a colonoscopy procedure?
Before a colonoscopy, your colon needs to be completely empty. Your doctor will provide instructions on how to prepare, which typically involves a clear liquid diet for a day or two before the procedure and taking a special laxative solution.
During the procedure, you will be sedated, and the doctor will insert a colonoscope (a long, flexible tube with a camera) into your rectum to examine your colon. The procedure usually takes about 30 minutes to an hour.

