Breast cancer remains the most prevalent cancer affecting women in Singapore, with statistics showing that over 2,000 women are diagnosed annually.
This alarming figure highlights the critical importance of regular breast screening.
The good news is that when detected early, breast cancer has exceptionally high cure rates, with patients potentially living cancer-free for decades after treatment.
The key to such positive outcomes lies in timely and appropriate breast screening.
This comprehensive guide explores everything you need to know about breast screening in Singapore, from understanding different screening methods to recognizing when and how often you should be screened based on your age and risk profile.
Related article: Health Screening in Singapore
Understanding Breast Cancer
Breast cancer develops when abnormal cells in breast tissue multiply uncontrollably, forming malignant tumors that can potentially spread to other parts of the body if left untreated.
What makes breast cancer particularly concerning is its silent progression—many women experience no noticeable symptoms during early stages.
The disease is especially prevalent in Singapore, where approximately 1 in 13 women will face a breast cancer diagnosis at some point in their lives.
This statistic underscores why regular screening has become a cornerstone of women’s healthcare in the country.
The Importance of Early Detection
Early detection dramatically increases treatment success rates. When breast cancer is identified at its earliest stages:
- Treatment options are more numerous and less invasive
- Recovery rates are significantly higher
- The chance of cancer recurrence decreases substantially
- Quality of life during and after treatment improves
Breast cancer screening plays a pivotal role in this early detection process by identifying abnormalities before they become symptomatic or before a lump grows large enough to be felt during self-examination.
You might be interested: Egg Freezing in Singapore
Common Breast Screening Methods
Mammogram: The Gold Standard
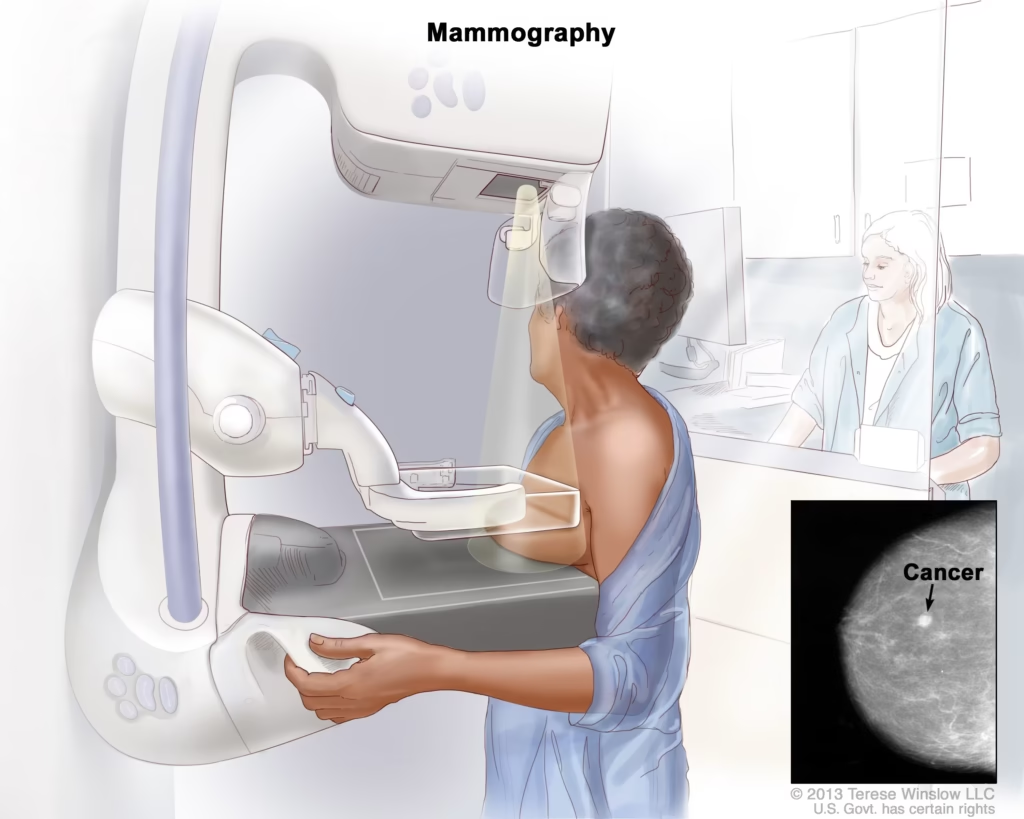
A mammogram is an X-ray examination of the breast tissue and remains the most reliable screening tool for early breast cancer detection. During this procedure:
- A female radiographer positions each breast between two flat plastic plates
- The breast tissue is compressed temporarily to obtain clearer images
- The procedure is performed separately on each breast
- Additional angles and magnified views may be taken if needed for closer examination
Mammograms excel at detecting tiny lumps and calcium deposits (microcalcifications) that may indicate early-stage breast cancer or non-cancerous conditions.
The radiation exposure during a mammogram is minimal—equivalent to about two months of exposure to natural background radiation—making the benefits far outweigh any potential risks.
It’s worth noting that mammogram accuracy can be affected by breast density. Younger women typically have denser breast tissue, which may sometimes obscure abnormalities on mammogram images.
You might like: HPV Vaccination in Singapore: A Comprehensive Guide
Breast Ultrasound: The Complementary Tool

A breast ultrasound employs sound waves to create images of breast tissue—the same technology used during pregnancy ultrasounds.
This non-invasive and painless procedure is particularly valuable for:
- Determining whether a detected lump is solid or fluid-filled (cystic)
- Providing clearer visualization of abnormalities in women with dense breast tissue
- Supplementing mammogram findings for more comprehensive assessment
Unlike mammograms, ultrasounds cannot detect microcalcifications, which can be early signs of breast cancer.
This limitation explains why ultrasounds typically complement rather than replace mammograms in a comprehensive screening approach.
This might be helpful: Endometriosis Treatment in Singapore
Magnetic Resonance Imaging (MRI)
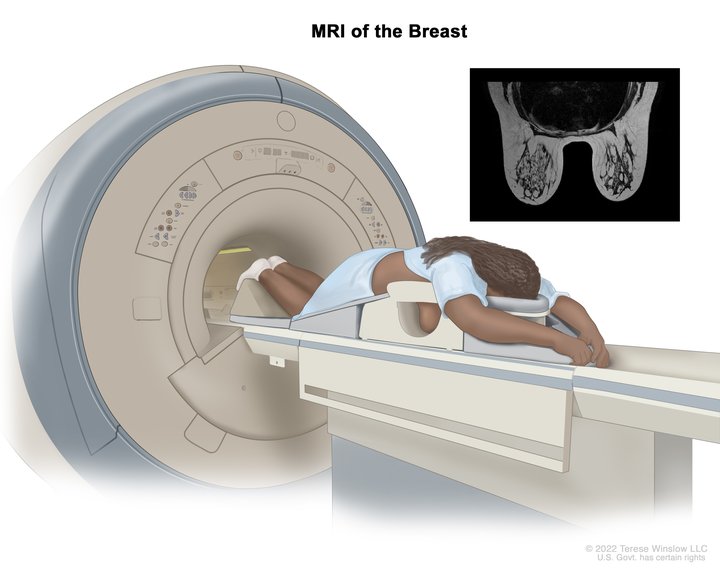
Breast MRI uses powerful magnets and radio waves to generate highly detailed images of breast tissue. While not typically used for routine screening, MRIs are recommended for:
- Women with a strong family history of breast cancer
- Women with known BRCA1 or BRCA2 gene mutations
- Women with very dense breast tissue where other screening methods may be less effective
- Women with breast implants that might obstruct clear mammogram imaging
MRI screenings can detect abnormalities that might be missed by other screening methods, making them particularly valuable for high-risk individuals.
You might be interested: The Ultimate Guide to Breast Augmentation in Singapore
Recommended Screening Guidelines by Age
The frequency and type of breast screening recommended varies according to age and individual risk factors:
Women Under 40
For women under 40 with average risk:
- Routine mammogram screening is generally not recommended
- Monthly breast self-examinations from age 18 onwards
- Annual clinical breast examinations by a healthcare professional
However, women with high breast cancer risk due to family history or genetic factors should consult specialists for personalized screening recommendations, which may include earlier and more frequent screenings.
Women Aged 40-49
For women in this age group:
- Annual mammogram screenings are recommended
- Monthly breast self-examinations
- Annual clinical breast examinations by a healthcare professional
- Supplementary ultrasound may be recommended, especially for those with dense breast tissue
This age group faces elevated breast cancer risk, justifying more frequent screenings despite younger age.
Related article: Menopause Treatment Singapore
Women Aged 50 and Above
For women over 50:
- Mammogram screenings every two years
- Monthly breast self-examinations
- Annual clinical breast examinations by a healthcare professional
- Additional screening methods as recommended by healthcare providers based on personal risk assessment
Breast Self-Examination: A Crucial Complement to Clinical Screening
Performing monthly breast self-examinations (BSE) helps women become familiar with the normal look and feel of their breasts, making it easier to identify changes that might warrant medical attention. The recommended BSE procedure includes:
- Visual Inspection
- Stand before a mirror with arms at your sides
- Raise arms above your head
- Press hands firmly on hips with chest muscles contracted
- Look for changes in breast size, shape, skin dimpling, or nipple changes
- Physical Examination While Lying Down
- Place a small pillow under the shoulder of the breast being examined
- Use the pads of your fingers to feel for lumps or thickening
- Examine the entire breast in smaller and smaller circles, starting from the outer edge
- Pay special attention to the area between the breast and armpit
- Examine the nipple area carefully
- Nipple Examination
- Gently squeeze each nipple to check for discharge or bleeding
Women should perform BSE approximately one week after menstruation starts, when breasts are least likely to be swollen or tender.
Post-menopausal women should choose a consistent day each month for examination.
You might like this: Hysterectomy in Singapore: Costs, Risks, Treatment
Subsidized Screening Programs in Singapore
The Singapore Health Promotion Board (HPB) offers the Screen For Life Breast Cancer Screening program, which provides subsidized mammogram screenings for eligible women. To qualify for this program:
- Women must be aged 50 and above, or between 40-49 with a doctor’s recommendation
- Women must not have had a mammogram within the past two years (for those over 50) or past year (for those 40-49)
- Women must not be experiencing breast symptoms such as painless lumps, nipple discharge, breast skin changes, etc.
Eligible women can access subsidized mammograms at participating screening centers verified by the Health Promotion Board and the Singapore Cancer Society.
Cost of Breast Cancer Screening in Singapore
The cost of breast screening varies depending on the screening method and healthcare facility:
| Screening Method | Approximate Cost Range (SGD) |
|---|---|
| Basic Mammogram | $100 – $200 |
| Digital Mammogram | $200 – $300 |
| Breast Ultrasound | $150 – $300 |
| Breast MRI | $800 – $1,500 |
Singaporean citizens and permanent residents can access subsidies through various government health initiatives, making screening more affordable.
It’s advisable to check with your healthcare provider about specific costs and whether your health insurance plan covers screening tests.
Understanding Breast Cancer Risk Factors
While regular screening is essential for all women, understanding risk factors can help individuals and healthcare providers determine the most appropriate screening protocol. Major risk factors include:
- Age: Risk increases with age, especially after menopause
- Family history: Having one or more close relatives diagnosed with breast cancer
- Personal history: Previous breast cancer diagnosis or certain non-cancerous breast conditions
- Genetic mutations: Particularly BRCA1 and BRCA2 gene mutations
- Early menstruation: Beginning menstruation before age 12
- Late menopause: Starting menopause after age 55
- Hormone therapy: Long-term use (more than five years) of combined hormone replacement therapy
- Lifestyle factors: Being overweight, physical inactivity, regular alcohol consumption
It’s important to note that having risk factors doesn’t guarantee developing breast cancer—many women with multiple risk factors never develop the disease.
Conversely, women with no apparent risk factors can still develop breast cancer, which is why regular screening remains essential for all women in the recommended age groups.
What Happens After Screening
Understanding Mammogram Results
After a mammogram, women typically receive one of the following results:
- Normal: No signs of breast cancer; continue with regular screening schedule
- Abnormal: Additional testing needed to determine whether cancer is present
An abnormal mammogram result doesn’t necessarily indicate cancer—it simply means further evaluation is necessary. Additional tests might include:
- Diagnostic mammogram (more detailed X-rays)
- Breast ultrasound
- Breast MRI
- Biopsy (removal of a small tissue sample for laboratory examination)
The Diagnostic Process
If additional tests suggest the presence of breast cancer, a biopsy will be performed to confirm the diagnosis. During staging, the extent of the disease is determined based on:
- Tumor size
- Lymph node involvement
- Whether cancer has spread to other parts of the body
- Presence of specific tumor markers (estrogen/progesterone receptors and HER2)
Based on these factors, breast cancer is typically classified into stages 0 through IV, which guide treatment planning.
Treatment Options for Breast Cancer
When breast cancer is diagnosed, several treatment approaches may be recommended based on cancer stage, type, and individual factors:
Surgical Interventions
Lumpectomy (Breast-Conserving Surgery)
- Removal of the tumor and a small margin of surrounding healthy tissue
- Typically followed by radiation therapy
- Preserves most breast tissue
- Results in minimal scarring and breast shape change
Mastectomy
- Surgical removal of the entire breast
- May include reconstruction options for women who desire them
- Skin-sparing and nipple-sparing techniques may be available depending on tumor location
- Reconstruction can use tissue from another part of the body or implants
Non-Surgical Treatments
Radiation Therapy
- Uses high-powered X-rays or protons to target and kill cancer cells
- Typically lasts between one to three weeks
- Often follows lumpectomy to eliminate any remaining cancer cells
Chemotherapy
- Administration of cancer-fighting drugs intravenously
- Reduces risk of cancer recurrence
- Side effects may include nausea, rash, fever, and hair loss
- Frequency and severity of side effects vary between patients
Hormone Therapy
- For cancers that are estrogen or progesterone receptor-positive
- Usually administered as a daily tablet
- Helps reduce the chance of cancer recurrence
- May be recommended for 5-10 years after primary treatment
Targeted Therapy
- For cancers with specific characteristics, such as HER2 overexpression
- Attacks specific cancer cell features while sparing healthy cells
- Can be administered orally or intravenously
Immunotherapy
- Utilizes the body’s immune system to fight cancer
- Not typically first-line treatment but may be used for rare cancers or recurrences
- One of the more expensive treatment options
Comprehensive FAQ Section
General Screening Questions
Q: At what age should I start breast cancer screening?
A: Women with average risk should begin annual mammograms at age 40.
Those with high risk due to family history or genetic factors should consult with specialists about starting earlier.
All women should practice monthly breast self-examinations starting at age 18.
Q: How often should I get a mammogram?
A: Women aged 40-49 should have annual mammograms, while women 50 and above can typically reduce frequency to once every two years.
However, your doctor may recommend a different schedule based on your personal risk profile.
Q: Is a mammogram painful?
A: Mammograms can cause temporary discomfort due to breast compression between the plates, but the procedure is not generally described as painful.
The compression lasts only a few seconds per image. If you experience significant discomfort, inform your radiographer who may be able to adjust the procedure for greater comfort.
Q: What’s the difference between screening and diagnostic mammograms?
A: Screening mammograms check for breast cancer in women with no symptoms, while diagnostic mammograms investigate specific concerns or abnormalities.
Diagnostic mammograms typically involve more images taken from additional angles compared to screening mammograms.
About Breast Cancer Risk
Q: Does not having any risk factors mean I won’t get breast cancer?
A: No, women without identified risk factors can still develop breast cancer. This is why regular screening is recommended for all women in the appropriate age groups, regardless of risk factors.
Q: My mother had breast cancer. Does that mean I’ll get it too?
A: Having a first-degree relative (mother, sister, daughter) with breast cancer increases your risk, but it doesn’t guarantee you’ll develop the disease.
Women with family history should discuss their specific risk profile with healthcare providers and may benefit from genetic counseling and testing.
Q: Does the radiation from mammograms increase my cancer risk?
A: The radiation exposure from mammograms is very low—equivalent to about two months of natural background radiation.
The benefits of early detection far outweigh the minimal risks associated with this level of radiation exposure.
Screening Procedures
Q: What’s the difference between a mammogram and a breast ultrasound?
A: Mammograms use X-rays to examine breast tissue and excel at detecting microcalcifications, while ultrasounds use sound waves to create images and are particularly useful for determining whether lumps are solid or fluid-filled (cystic).
Ultrasounds cannot detect microcalcifications, which is why they typically complement rather than replace mammograms.
Q: Should I get a breast MRI instead of a mammogram?
A: For most women, mammograms remain the standard screening tool.
Breast MRIs are typically reserved for women at high risk of breast cancer or those with dense breast tissue where mammograms may be less effective.
Your doctor can advise whether an MRI would be beneficial in your specific case.
Q: What should I do to prepare for a mammogram?
A: Schedule your mammogram for the week after your menstrual period when breasts are less tender.
On the day of the examination, avoid using deodorants, antiperspirants, powders, or lotions on your breasts or underarms, as these can appear as calcium spots on the X-ray.
Wear a two-piece outfit for easy changing, and consider taking an over-the-counter pain reliever an hour before the appointment if you’ve experienced discomfort during previous mammograms.
After Screening
Q: What happens if my mammogram shows an abnormality?
A: An abnormal mammogram result doesn’t necessarily indicate cancer; many abnormalities are non-cancerous.
Your doctor will likely recommend additional tests such as a diagnostic mammogram, ultrasound, or possibly a biopsy to determine the nature of the abnormality.
Q: How long does it take to get mammogram results?
A: Results typically become available within 1-2 weeks. Many facilities now offer online portals where you can access your results as soon as they’re available.
If there are concerns requiring immediate attention, you’ll likely be contacted sooner.
Q: What are the survival rates for breast cancer detected through screening?
A: When breast cancer is detected early through screening, five-year survival rates exceed 90%.
This high survival rate underscores the importance of regular screening for early detection.
Subsidized Screening Programs
Q: How do I qualify for subsidized mammogram screening in Singapore?
A: To qualify for subsidized screening under the Screen For Life program, you must be a Singapore citizen or permanent resident aged 50 and above (or between 40-49 with a doctor’s recommendation).
You should not have had a mammogram within the past two years (for those over 50) or past year (for those 40-49), and you must not be experiencing breast symptoms.
Q: Where can I get a subsidized mammogram in Singapore?
A: Subsidized mammograms are available at participating Breast Screening Centers verified by the Health Promotion Board and the Singapore Cancer Society.
A complete list of participating centers can be found on the HPB website or obtained from polyclinics and community health centers.
Q: What if I can’t afford a mammogram even with subsidies?
A: Additional financial assistance programs are available for eligible low-income women through the Singapore Cancer Society and various community assistance funds.
Speak with social workers at polyclinics or public hospitals about available options.
Conclusion
Breast cancer screening plays a crucial role in women’s health, particularly in Singapore where breast cancer rates continue to rise.
Regular screening through mammograms, supplemented by breast ultrasounds when appropriate, offers the best opportunity for early detection and successful treatment.
The Singapore government has made significant efforts to increase screening accessibility through subsidized programs, recognizing that early detection not only saves lives but also reduces the overall healthcare burden associated with advanced-stage breast cancer treatment.
Every woman should prioritize regular breast screening according to recommended guidelines based on her age and risk profile.
Equally important is becoming familiar with how your breasts normally look and feel through monthly self-examinations, allowing you to notice changes promptly and seek medical attention when needed.
Remember that breast cancer, when detected early, has excellent treatment outcomes.
Don’t let fear or inconvenience prevent you from taking this critical step toward protecting your health. Schedule your breast screening today—it could save your life.

