Cushing syndrome represents a complex hormonal disorder that requires specialized medical attention and personalized treatment approaches.
This comprehensive guide explores the condition in detail, with a focus on available treatment options, diagnostic methods, and long-term management strategies.
Understanding Cushing Syndrome
Cushing syndrome is a hormonal disorder characterized by prolonged exposure to excessive levels of cortisol, commonly known as the “stress hormone.”
This condition disrupts normal bodily functions across multiple systems, leading to distinctive physical and metabolic changes.
While rare—affecting only 40 to 70 people per million annually—Cushing syndrome requires prompt medical intervention to prevent serious complications.
Read more: Which Endocrinologist in Singapore Should You Consider?
What Causes Cushing Syndrome?
The elevated cortisol levels associated with Cushing syndrome can stem from several sources, generally categorized as endogenous (internal) or exogenous (external).
Endogenous Causes originate within the body. Pituitary adenomas, known as Cushing Disease, account for approximately 70% of cases where benign tumors in the pituitary gland produce excess adrenocorticotropic hormone (ACTH), stimulating the adrenal glands to overproduce cortisol.
Adrenal tumors, both benign adenomas and malignant carcinomas, can directly produce excess cortisol, bypassing normal regulatory mechanisms.
Ectopic ACTH production occurs when non-pituitary tumors, typically found in the lungs (small cell lung carcinoma) or pancreas (carcinoid tumors), secrete ACTH, leading to increased cortisol production.
In rare cases, genetic conditions such as Multiple Endocrine Neoplasia Type 1 (MEN1) can predispose individuals to tumors that cause Cushing syndrome.
Exogenous Causes come from outside sources, primarily through long-term use of corticosteroid medications such as prednisone or dexamethasone.
These medications, prescribed for treating inflammatory conditions, autoimmune disorders, or after organ transplantation, represent the most common overall cause of Cushing syndrome.
Related article: Diabetes Treatment in Singapore: Types, Risks
Clinical Manifestations of Cushing Syndrome
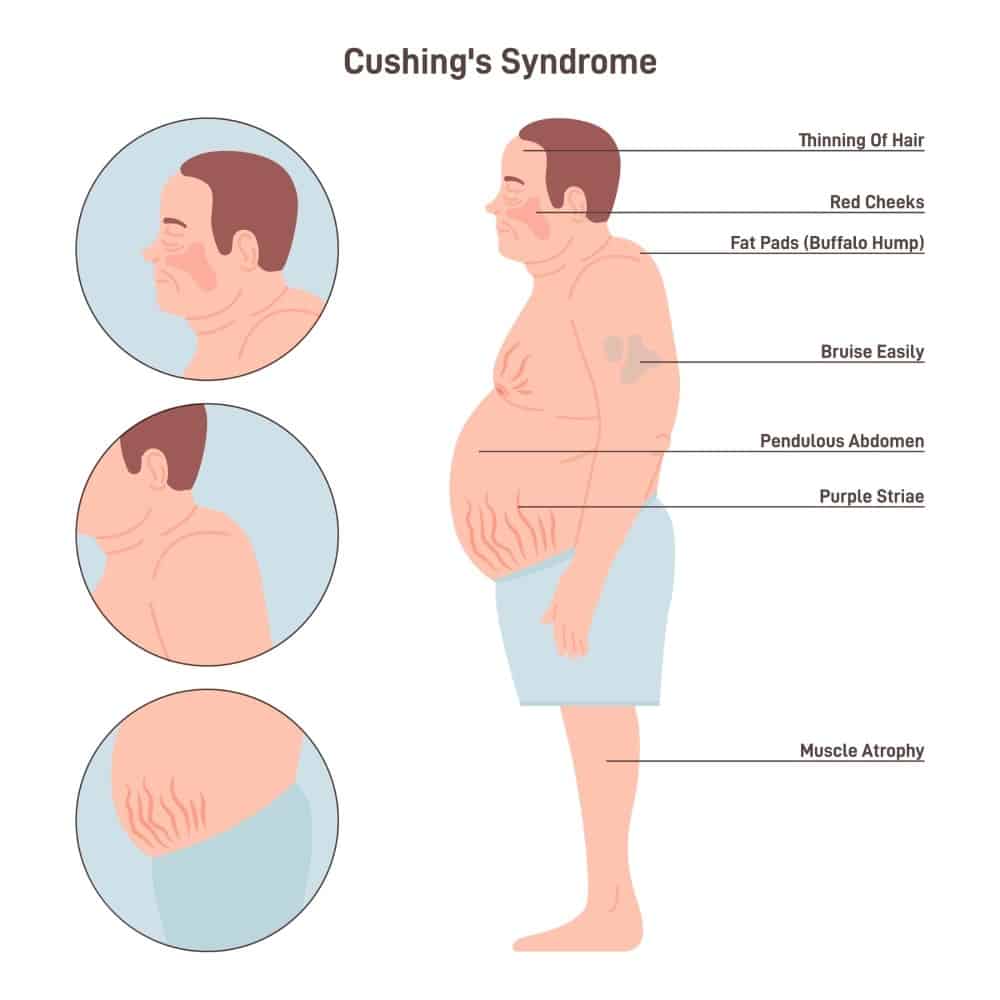
Patients with Cushing syndrome typically develop a characteristic constellation of symptoms that may appear gradually over time.
These symptoms affect multiple body systems and can significantly impact quality of life.
Distinctive Physical Changes
Cushing syndrome produces characteristic physical alterations that often prompt medical evaluation.
The distinctive weight distribution pattern includes central obesity with thin limbs, creating a body shape featuring increased fat deposits in the face (“moon face”), between the shoulders (“buffalo hump”), and in the abdomen.
Skin undergoes significant changes, becoming thin and fragile, bruising easily and healing poorly. Purple or pink stretch marks (striae) commonly develop on the abdomen, thighs, breasts, and arms, accompanied by facial plethora (redness).
Musculoskeletal effects include muscle wasting and weakness, particularly in the extremities, along with decreased bone density that leads to osteoporosis and heightened fracture risk.
Gender-specific changes often occur, with women experiencing excess facial and body hair growth (hirsutism) and acne, while men may encounter decreased libido and erectile dysfunction.
Related article: Gestational Diabetes Treatment in Singapore
Metabolic and Systemic Manifestations
Cushing syndrome affects multiple body systems beyond visible physical changes.
Cardiovascular complications include hypertension and increased risk of heart disease, often requiring ongoing management.
Glucose metabolism becomes disrupted, with elevated blood glucose levels, insulin resistance, and increased risk of developing diabetes.
Immune function weakens considerably, leading to frequent and persistent infections, particularly fungal infections that may be difficult to resolve.
The reproductive system experiences significant disruption, with women commonly experiencing menstrual irregularities or complete cessation of menstruation, while men may have reduced fertility.
Related article: Comprehensive Guide to Coronary Angioplasty in Singapore
Psychological and Cognitive Effects
The impact of cortisol excess extends to brain function, causing notable psychological and cognitive changes.
Mood disturbances manifest as depression, anxiety, irritability, and unpredictable mood swings that can significantly affect quality of life.
Cognitive function often declines, with patients reporting difficulty concentrating, memory problems, and disturbed sleep patterns that further compound mental health challenges.
Diagnostic Approach to Cushing Syndrome
Diagnosing Cushing syndrome requires a systematic approach combining clinical evaluation with biochemical testing and imaging studies.
The diagnostic process often begins with identifying characteristic symptoms and proceeds through several stages of confirmation.
Read more: Diabetes Myths Debunked: Separating Fact from Fiction
Initial Biochemical Testing
The cornerstone of diagnosis is the 24-hour urinary free cortisol test, which measures cortisol excretion over a full day, providing a comprehensive view of overall cortisol production.
Multiple collections may be necessary as levels can fluctuate daily.
Late-night salivary cortisol testing offers valuable insights, as cortisol follows a diurnal rhythm with levels normally lowest at night.
Elevated midnight salivary cortisol levels suggest disruption of this natural rhythm, a hallmark of Cushing syndrome.
Dexamethasone suppression tests play a crucial role in diagnosis.
The low-dose test involves administering 1-2 mg dexamethasone at night, which should suppress morning cortisol in healthy individuals but fails to do so in Cushing syndrome.
The high-dose version helps differentiate between pituitary and non-pituitary sources of ACTH production.
Additionally, plasma ACTH measurement helps determine if excess cortisol is ACTH-dependent or independent.
Undetectable levels suggest an adrenal cause, while high levels indicate either a pituitary or ectopic source.
You might be interested: Type 2 Diabetes Treatment in Singapore: Symptoms, Risks
Advanced Diagnostic Methods
When initial tests suggest Cushing syndrome, imaging studies become necessary to identify the source.
MRI or CT of the pituitary can detect pituitary microadenomas in cases of Cushing disease, while CT or MRI of adrenal glands identifies adrenal tumors.
Chest and abdominal imaging may locate potential ectopic ACTH-producing tumors when suspected.
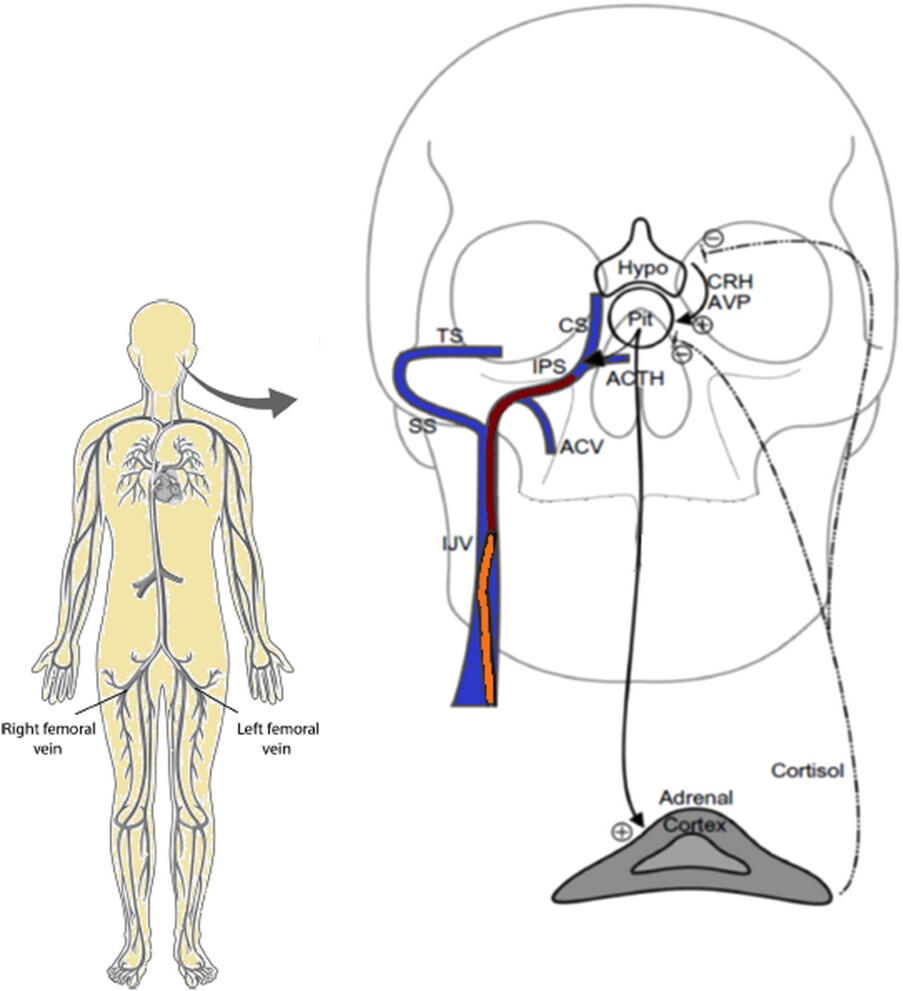
For challenging cases, bilateral inferior petrosal sinus sampling (BIPSS) offers definitive insights.
This specialized procedure measures ACTH from veins draining the pituitary to confirm a pituitary origin of ACTH production with remarkably high accuracy (95-98%), helping differentiate between pituitary and ectopic sources when other tests yield inconclusive results.
You might like: Pituitary Gland Disorders Treatment in Singapore: Symptoms, Causes
Treatment Strategies for Cushing Syndrome
Treatment approaches for Cushing syndrome depend on the underlying cause and aim to normalize cortisol levels while addressing complications.
A multidisciplinary approach involving endocrinologists, neurosurgeons, and other specialists is essential for optimal outcomes.
Surgical Interventions
Surgery remains the first-line treatment for most forms of endogenous Cushing syndrome.
For pituitary adenomas, transsphenoidal surgery involves accessing the pituitary gland through the nasal cavity and sphenoid sinus.
This approach offers a high success rate (70-90%) for microadenomas when performed by experienced surgeons, though patients may require hormone replacement therapy post-surgery until the hypothalamic-pituitary-adrenal (HPA) axis recovers.
Adrenalectomy serves as the primary intervention for adrenal tumors.
The laparoscopic approach is preferred for benign adenomas, offering minimal invasiveness and faster recovery.
Open surgery may be necessary for larger tumors or adrenocortical carcinomas.
In cases of bilateral adrenal hyperplasia, bilateral adrenalectomy might be required, which necessitates lifelong glucocorticoid replacement therapy to compensate for the loss of adrenal function.
For ectopic ACTH sources, surgical resection of the non-pituitary tumor producing ACTH represents the optimal approach.
The success of this intervention depends on accurate tumor identification and accessibility, which varies by tumor type and location.
Medication-Based Treatments
Medications play a crucial role, particularly when surgery is contraindicated, unsuccessful, or as adjunctive therapy.
Cortisol-lowering medications include steroidogenesis inhibitors such as ketoconazole, which blocks several steps in cortisol synthesis but requires liver function monitoring;
Metyrapone, which inhibits 11-beta-hydroxylase enzyme but may cause hirsutism and acne in women;
Mitotane, a potent adrenolytic agent primarily used for adrenocortical carcinoma that requires careful monitoring due to serious side effects; and
Osilodrostat, a newer agent that inhibits 11-beta-hydroxylase and is specifically approved for Cushing syndrome.
Pituitary-directed therapies include pasireotide, a somatostatin analog that suppresses ACTH production but may cause hyperglycemia, and cabergoline, a dopamine agonist that may reduce ACTH secretion in some pituitary tumors.
Glucocorticoid receptor antagonists like mifepristone block cortisol action at its receptor, proving useful for managing metabolic complications but challenging to monitor as they don’t reduce cortisol levels.
In emergency situations with severe, life-threatening cases requiring rapid control, etomidate serves as an intravenous anesthetic with cortisol-blocking properties that can quickly reduce dangerously high cortisol levels.
Radiation Therapy
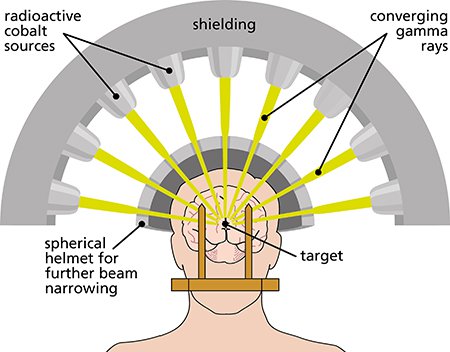
Radiation therapy serves as an alternative or adjunctive treatment when surgery is unsuccessful or contraindicated.
Conventional radiotherapy delivers fractionated doses over approximately six weeks, though its effects may take months to years to fully manifest.
This approach may cause hypopituitarism requiring hormone replacement therapy as a side effect.
Stereotactic radiosurgery offers a more targeted approach, delivering a single high-dose focused radiation treatment (using technologies such as Gamma Knife or proton beam therapy).
This method provides more precise targeting with potentially fewer complications and is particularly useful for well-defined, smaller tumors that can be clearly visualized and targeted.
Managing Exogenous Cushing Syndrome
For iatrogenic Cushing syndrome caused by medical treatment with glucocorticoids, management centers on carefully adjusting medication regimens.
Glucocorticoid tapering involves gradual dose reduction under close medical supervision.
Abrupt discontinuation must be avoided as it can precipitate potentially life-threatening adrenal crisis.
Clinicians may implement alternative day dosing schedules or substitute lower-potency glucocorticoids when possible.
Exploring non-glucocorticoid alternatives for treating the underlying condition represents another important strategy.
This might include using non-steroid options for inflammatory or autoimmune conditions, or implementing localized rather than systemic steroid delivery methods when feasible to minimize systemic absorption and effects.
Long-Term Management and Follow-Up
Recovery from Cushing syndrome requires ongoing medical supervision and supportive care:
Monitoring and Surveillance
- Regular assessment of cortisol levels to detect potential recurrence.
- Screening for and managing complications (diabetes, hypertension, osteoporosis).
- Periodic imaging studies for patients with tumors to detect regrowth.
Supportive Therapies
- Bone Health Management:
- Calcium and vitamin D supplementation.
- Bisphosphonates or other bone-protective medications if osteoporosis is present.
- Weight-bearing exercise as strength permits.
- Cardiovascular Risk Reduction:
- Blood pressure management.
- Lipid-lowering interventions as needed.
- Lifestyle modifications for heart health.
- Metabolic Optimization:
- Blood glucose monitoring and management.
- Dietary counseling appropriate to metabolic status.
Psychological Support
- Counseling for body image concerns and mood disturbances.
- Support groups for patients with rare endocrine disorders.
- Cognitive behavioral therapy for persistent psychological symptoms.
Special Considerations for Treatment in Singapore
Singapore offers advanced medical facilities with expertise in treating complex endocrine disorders like Cushing syndrome:
- Specialized Centers:
- Major hospitals like Singapore General Hospital, National University Hospital, and Mount Elizabeth Hospital have dedicated endocrinology departments experienced in managing Cushing syndrome.
- Multidisciplinary teams including endocrinologists, neurosurgeons, and radiologists coordinate care.
- Advanced Diagnostic Capabilities:
- State-of-the-art imaging technologies including high-resolution MRI and PET scanning.
- Comprehensive hormonal testing and specialized nuclear medicine studies.
- Surgical Expertise:
- Experienced pituitary surgeons trained in minimally invasive techniques.
- Advanced laparoscopic and robotic surgical options for adrenal tumors.
- Treatment Accessibility:
- Availability of newer medications like osilodrostat and pasireotide.
- Access to stereotactic radiosurgery and advanced radiation therapy modalities.
- Long-term Follow-up:
- Comprehensive monitoring programs for patients after treatment.
- Digital health platforms enabling remote monitoring for appropriate patients.
Recovery and Prognosis
The recovery trajectory for Cushing syndrome varies depending on the cause, treatment approach, and individual factors:
- Post-Surgical Recovery:
- Initial recovery from pituitary or adrenal surgery typically takes 4-6 weeks.
- Hormonal normalization may require months.
- Some patients experience a temporary period of adrenal insufficiency requiring hormone replacement.
- Long-term Outlook:
- Successful treatment can reverse many, though not all, physical changes.
- Metabolic improvements (blood pressure, glucose levels) often occur within weeks to months.
- Bone density recovery takes longer, sometimes years.
- Psychological symptoms typically improve but may persist in some patients.
- Recurrence Risk:
- Approximately 10% of patients with Cushing disease experience recurrence within a decade after successful treatment.
- Regular monitoring with cortisol testing helps detect recurrence early.
Prevention and Health Maintenance
While primary prevention of endogenous Cushing syndrome is not possible, certain measures can reduce risks associated with exogenous causes and improve outcomes:
- Medication Management:
- For patients requiring long-term corticosteroid therapy, using the lowest effective dose for the shortest duration necessary.
- Considering alternative-day dosing schedules when possible.
- Regular medical monitoring for early detection of Cushing’s features.
- Lifestyle Modifications:
- Regular physical activity appropriate to strength and capability.
- Balanced diet rich in calcium and protein.
- Smoking cessation and limited alcohol consumption.
- Preventive Screening:
- Bone density assessment.
- Cardiovascular risk evaluation.
- Psychological health monitoring.
Frequently Asked Questions
What is the difference between Cushing syndrome and Cushing disease?
Cushing syndrome is the broad term for conditions characterized by excess cortisol from any source, while Cushing disease specifically refers to Cushing syndrome caused by a pituitary adenoma producing excess ACTH.
Essentially, Cushing disease is a specific type of Cushing syndrome, accounting for approximately 70% of endogenous cases in adults and 60-70% in children and adolescents.
How long does recovery from Cushing syndrome take?
Recovery timelines vary significantly depending on the cause, treatment approach, and individual factors.
Generally, initial recovery from surgery takes 4-6 weeks, but hormonal normalization may require months.
Physical changes like weight redistribution gradually improve over 6-12 months. Bone density recovery takes longer, often years.
Some patients experience a temporary period of adrenal insufficiency requiring hormone replacement.
Complete resolution of all symptoms may take 12-18 months or longer in some cases.
Can Cushing syndrome recur after successful treatment?
Yes, Cushing syndrome can recur even after successful initial treatment.
Approximately 10% of patients with Cushing disease experience recurrence within a decade.
Recurrence rates vary by cause: pituitary adenomas have a 10-15% recurrence rate, adrenal tumors rarely recur if completely removed, and ectopic sources may recur depending on the underlying tumor biology.
This necessitates long-term follow-up with regular cortisol testing to detect any recurrence early, allowing for prompt intervention.
How is Cushing syndrome diagnosed if symptoms are subtle?
Diagnosing subtle or early Cushing syndrome presents challenges and typically requires a stepwise approach.
Clinicians begin with screening tests like 24-hour urinary free cortisol measurement, late-night salivary cortisol testing, or the overnight dexamethasone suppression test.
Multiple tests are often necessary as results can be indeterminate in mild cases.
If screening tests suggest Cushing syndrome, further testing to determine the cause includes plasma ACTH levels, high-dose dexamethasone suppression tests, and imaging studies.
In challenging cases, petrosal sinus sampling may be required for definitive diagnosis.
What medications are used to treat Cushing syndrome?
Several medication classes are employed in treating Cushing syndrome.
Steroidogenesis inhibitors block cortisol production at different enzymatic steps and include ketoconazole (400-1200 mg daily), metyrapone (500 mg to 6 g daily), mitotane (primarily for adrenocortical carcinoma), osilodrostat (a newer approved medication), and levoketoconazole (up to 1200 mg daily).
Pituitary-directed medications aim to reduce ACTH production and include pasireotide (a somatostatin analog) and cabergoline (a dopamine agonist).
Glucocorticoid receptor antagonists like mifepristone block cortisol action at cellular receptors rather than reducing hormone levels.
For emergencies with dangerously high cortisol levels, intravenous etomidate can rapidly bring levels down.
The choice of medication depends on the underlying disease cause, symptom severity, presence of comorbidities, and whether the treatment is being used as primary therapy, adjunctive therapy, or for recurrence management.
What happens if Cushing syndrome is left untreated?
Untreated Cushing syndrome can lead to serious, potentially life-threatening complications.
Cardiovascular problems develop and worsen, including persistent hypertension, heart failure, stroke, and increased risk of blood clots such as deep vein thrombosis and pulmonary embolism.
Metabolic disturbances progress, resulting in more severe diabetes with complications, dangerous electrolyte imbalances (particularly hypokalemia), and metabolic acidosis.
Skeletal deterioration accelerates without intervention, leading to severe osteoporosis, multiple fractures, vertebral compression, and chronic pain that significantly impacts mobility and quality of life.
Immunosuppression becomes more pronounced, resulting in recurrent and severe infections, including opportunistic infections that can become life-threatening particularly in advanced cases.
Neuropsychiatric manifestations worsen over time, including deepening depression, potential psychosis, cognitive decline, and increased suicide risk.
Overall mortality is significantly increased in untreated cases, with studies indicating a 5-year survival rate of only 50% in severe cases without intervention.
The complex interplay of these complications makes early diagnosis and comprehensive treatment essential for preserving health and longevity.
How does radiation therapy work for treating Cushing syndrome?
Radiation therapy for Cushing syndrome targets the source of excessive hormone production, most commonly pituitary adenomas. There are two main approaches:
- Conventional fractionated radiotherapy delivers multiple smaller doses over 5-6 weeks. Radiation damages the DNA of rapidly dividing tumor cells, eventually leading to their death while attempting to minimize damage to surrounding tissues. Effects develop gradually, with hormonal improvements taking months to years.
- Stereotactic radiosurgery (like Gamma Knife or CyberKnife) delivers a single focused high dose of radiation precisely to the tumor. This technique offers greater precision for well-defined, smaller tumors and potentially faster results.
Both methods may cause hypopituitarism requiring hormone replacement therapy.
Radiation is typically used when surgery is unsuccessful or contraindicated, or for recurrent disease.
Regular follow-up monitoring is essential as effects develop gradually and may continue to evolve for years after treatment.
What dietary recommendations should patients with Cushing syndrome follow?
Patients with Cushing syndrome benefit from specific dietary approaches that address the metabolic complications associated with excess cortisol.
A calcium and vitamin D-rich diet incorporating dairy products, fortified plant milks, leafy greens, and fatty fish helps combat bone density loss that commonly occurs.
Adequate protein intake (approximately 0.8-1.0 g/kg body weight) supports muscle maintenance during periods of cortisol-induced muscle wasting, which is particularly important for preserving functional capacity.
Sodium restriction helps manage hypertension and fluid retention common in Cushing syndrome, while emphasizing potassium-rich foods such as bananas, oranges, potatoes, and leafy greens can help address hypokalemia that sometimes occurs.
Focusing on low glycemic index carbohydrates—whole grains, legumes, and non-starchy vegetables—helps manage the insulin resistance and glucose intolerance that frequently accompany the condition.
Anti-inflammatory foods containing omega-3 fatty acids (fatty fish, walnuts, flaxseeds) and antioxidant-rich fruits and vegetables may help counteract some inflammatory effects of excess cortisol.
However, individualized nutrition counseling is strongly recommended, as dietary needs may vary significantly based on specific complications, medication effects, and stage of treatment.
What psychological support is available for patients with Cushing syndrome?
The psychological impact of Cushing syndrome is significant, requiring comprehensive support on multiple fronts.
Clinical psychology and psychiatry services provide professional mental health support addressing depression, anxiety, body image concerns, and cognitive changes directly associated with the condition and its treatment.
Cognitive Behavioral Therapy (CBT) has proven particularly effective for addressing negative thought patterns and developing coping strategies for body image concerns and mood disturbances that persist even after biochemical control is achieved.
Connecting with others experiencing similar challenges through support groups provides validation and practical coping strategies that complement medical care.
Both in-person and online groups are available, allowing patients to choose formats that best suit their comfort level and practical circumstances.
Family therapy helps loved ones understand the condition and its psychological effects, improving the support system for the patient during the challenging treatment and recovery process.
Neuropsychological assessment may be beneficial for evaluating and addressing cognitive changes that can occur with prolonged cortisol excess.
Rehabilitation psychology supports adaptation to physical limitations during recovery and helps develop strategies to manage any persistent challenges.
In Singapore, these psychological support services are readily available through hospital psychology departments, specialized endocrine clinics, and community mental health services that can be integrated into comprehensive care plans.

