Understanding Diabetes Mellitus
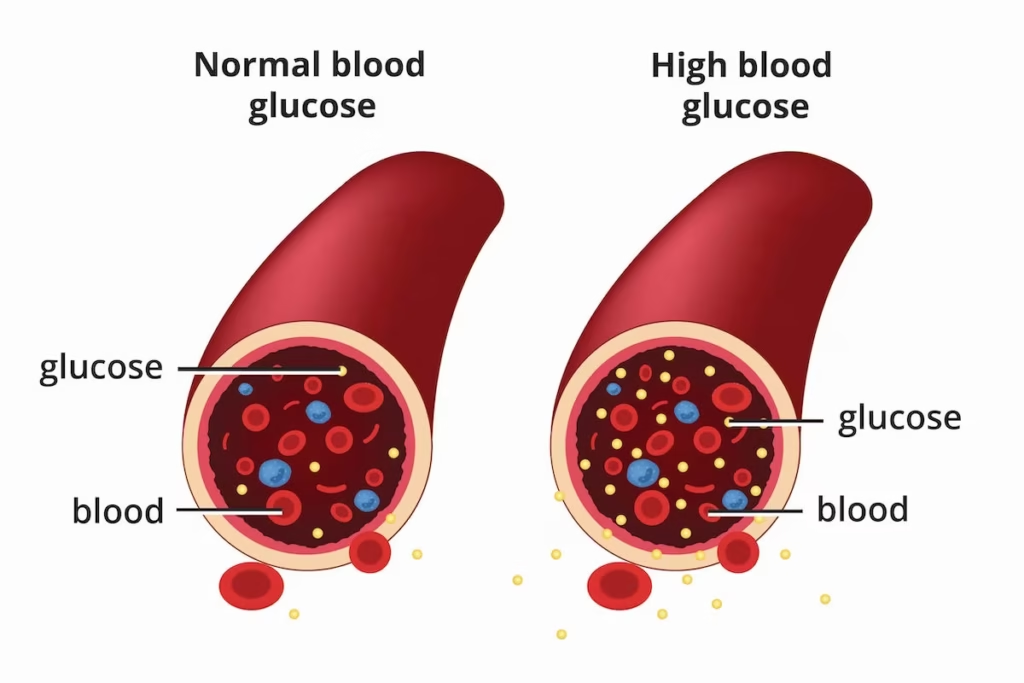
Diabetes mellitus is a chronic metabolic disorder characterized by the body’s inability to properly regulate blood glucose levels.
This condition occurs either when the pancreas cannot produce sufficient insulin or when the body cannot effectively use the insulin it produces.
Insulin is crucial as it regulates the transfer of glucose from the bloodstream into body cells.
For people with diabetes, insufficient insulin production or utilization results in elevated blood glucose levels, known as hyperglycemia.
According to the International Diabetes Federation, approximately 230 million people worldwide have diabetes, and this number is projected to increase to 350 million by 2025.
In Singapore specifically, about 1 in 10 Singaporeans live with diabetes, with this ratio increasing to 1 in 3 for those above 60 years of age. Alarmingly, the Ministry of Health (MOH) estimates that about one-third of diabetics in Singapore are unaware of their condition.
Read more: Which Endocrinologist in Singapore Should You Consider?
Types of Diabetes

There are three main types of diabetes:
Type 1 Diabetes
Type 1 diabetes typically develops rapidly and often at a young age, though it can affect individuals of any age. In this form of diabetes, the pancreas does not produce sufficient insulin, requiring daily insulin administration.
While symptoms may not be apparent initially, they tend to manifest suddenly. Type 1 diabetes accounts for approximately 5-10% of all diabetes cases.
Read more: Type 1 Diabetes Treatment in Singapore: Causes, Risks
Type 2 Diabetes
Type 2 diabetes is the most prevalent form in Singapore. It develops gradually and is more common among sedentary and overweight individuals.
This type occurs due to the body’s inability to effectively use insulin to facilitate cell processes and generate energy.
There is often a genetic predisposition, with Type 2 diabetes running in families. Lifestyle factors such as poor diet, lack of exercise, and excess weight significantly contribute to its development.
Read more: Type 2 Diabetes Treatment in Singapore: Symptoms, Risks
Gestational Diabetes
Gestational diabetes occurs during pregnancy when blood glucose levels rise above normal but are not high enough for a diabetes diagnosis.
Women with gestational diabetes face increased risks of complications during pregnancy and childbirth. Both these women and their children may be more susceptible to developing Type 2 diabetes later in life.
More information: Gestational Diabetes Treatment in Singapore
Diabetes and Cardiovascular Health
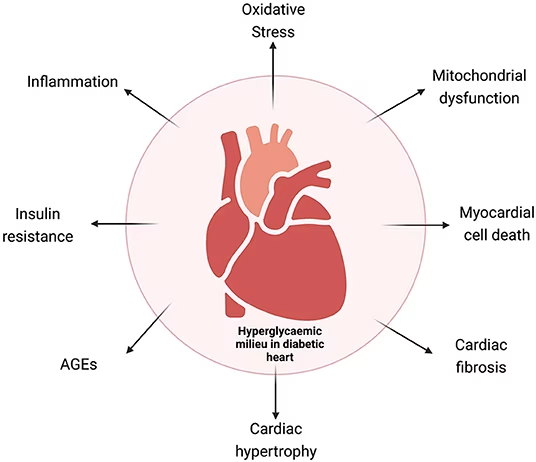
People with diabetes are two to four times more likely to develop coronary artery disease and stroke compared to those without diabetes. Diabetes is frequently associated with other cardiovascular risk factors, including:
- High blood pressure
- Elevated total cholesterol and triglyceride levels
- Decreased HDL (High-Density Lipoprotein) cholesterol levels
- Obesity
Insulin resistance, a condition where the body does not respond efficiently to insulin, can predispose individuals to both diabetes mellitus and cardiovascular disease. Both Type 1 and Type 2 diabetes significantly increase the risk of cardiovascular complications.
This might help: Diabetes Myths Debunked: Separating Fact from Fiction
Recognizing Diabetes Symptoms
Early recognition of diabetes symptoms is crucial for timely intervention. Some common signs and symptoms include:
- Dry mouth
- Blurred vision
- Extreme fatigue
- Slow-healing sores or cuts
- Consistently feeling hungrier than usual
- Tingling, pain, or numbness in the hands/feet
- Frequent urination
- Unexplained weight loss
- Increased thirst
It’s important to note that diabetes can be a “silent” disease in its early stages, with symptoms not appearing until complications develop. This underscores the importance of regular screening, especially for those at higher risk.
Related article: Pituitary Gland Disorders Treatment in Singapore: Symptoms, Causes
Diabetes Risk Factors in Singapore
Several factors increase the risk of developing diabetes:
Age
Adults aged 45 and above face increased risk due to insulin resistance and declining pancreatic function that naturally occur with aging.
Body Mass Index (BMI)
Individuals with a BMI of 23 and above have a higher risk, particularly those leading sedentary lifestyles.
Family History
Those with a family history of diabetes are at greater risk, especially when combined with a sedentary lifestyle.
Pre-diabetes
Individuals diagnosed with pre-diabetes (higher than normal blood glucose levels) are at risk of developing Type 2 diabetes, as well as heart attacks and stroke if their condition worsens due to poor management.
You might like: Cushing Syndrome Treatment: Causes, Symptoms
Diabetes Screening and Diagnosis in Singapore
Early detection through proper screening is vital for effective diabetes management. In Singapore, there are four primary tests used for diabetes diagnosis:
Fasting Blood Sugar Test
This test requires an overnight fast of at least eight hours before blood sampling. A result of ≥ 7.0 mmol/L indicates diabetes.
Casual Blood Sugar Test
Similar to the fasting test but without the need for fasting. A result of ≥ 11.1 mmol/L suggests diabetes.
Glycated Hemoglobin (HbA1C) Test
This test can be conducted via a traditional blood draw or as a point-of-care test requiring only a finger prick, with results available in about 15 minutes. An HbA1c level of ≥ 7.0% typically indicates diabetes.
Oral Glucose Tolerance Test (OGTT)
This comprehensive test involves fasting overnight, followed by drinking a sugary solution at the healthcare provider’s office. Blood sugar levels are tested before consumption and two hours after. A result of ≥ 11.1 mmol/L after two hours suggests diabetes.
The Singapore HbA1c guidelines interpret results as follows:
| HbA1c Level | Interpretation | Recommended Action | Diagnosis |
|---|---|---|---|
| 6.0% and below | Low probability of diabetes | No further tests needed if asymptomatic; further testing if symptoms present | No Diabetes |
| 6.1% to 6.9% | Further testing required | Proceed to Fasting Glucose test or OGTT | Pre-diabetes / Increased risk |
| 7.0% and above | High probability of diabetes | No further tests needed | Diabetes |
Most general practice (GP) clinics in Singapore can perform blood sampling for these tests. Additionally, subsidized screening is available through various programs:
- For those aged 18-39: Take the Diabetes Risk Assessment (DRA) to determine risk level
- For those aged 40 and above: Subsidized blood glucose tests under Screen for Life at $5 or less
Comprehensive Diabetes Management
Effective diabetes management involves a multifaceted approach combining medical treatment with lifestyle modifications:
Lifestyle Modifications
1. Balanced Diet
Effective diabetes management begins with making informed dietary choices that help maintain stable blood glucose levels.
Patients should avoid foods high in cholesterol and saturated fats, including animal fats, whole milk products, eggs, red meat, coconut milk, and palm oil, as these can worsen insulin resistance and cardiovascular risk factors.
Instead, individuals should choose lean meat, fish, and low-fat dairy products, which provide essential nutrients without excessive saturated fat content.
Increasing intake of fruits, non-starchy vegetables, and whole grains provides important fiber, vitamins, and minerals while helping to stabilize blood sugar levels throughout the day.
Limiting sugar consumption by opting for less sweet foods and drinks is crucial for preventing blood glucose spikes that can complicate diabetes management.
Many patients benefit from carbohydrate counting, which involves tracking the amount of carbohydrates consumed at each meal to better predict and manage blood glucose responses.
Aiming for smaller, portion-controlled meals with a regular eating schedule helps maintain steady blood glucose levels and prevents dramatic fluctuations that can occur with irregular eating patterns.
This approach also supports weight management and helps the body develop predictable insulin needs throughout the day.
2. Regular Exercise
Physical activity plays a fundamental role in diabetes management by improving insulin sensitivity and glucose uptake by muscles.
Patients should exercise at least three times a week, with walking being one of the most accessible and effective forms of physical activity for people with diabetes.
Adults should aim for 30 minutes or more of moderate aerobic exercise most days of the week, totaling at least 150 minutes weekly, which has been shown to significantly improve glycemic control and cardiovascular health.
Children with diabetes should engage in 60 minutes of moderate to vigorous aerobic exercise daily to support healthy growth and development while maintaining optimal blood glucose control.
Incorporating resistance exercises such as weightlifting, yoga, and calisthenics helps build and maintain muscle mass, which is important for glucose metabolism and overall strength.
Breaking up long periods of inactivity by taking brief movement breaks every 30 minutes can help prevent blood glucose spikes that often occur during prolonged sitting, making this strategy particularly important for individuals with sedentary jobs or lifestyles.
3. Weight Management
Maintaining a healthy weight is essential for optimal diabetes management and overall health outcomes. Patients can calculate their Body Mass Index (BMI) using the formula:
Weight in kilograms divided by height in meters squared, with a healthy BMI range falling between 18.5 and 22.9 for most adults.
The waist-to-hip ratio, calculated by dividing waist circumference by hip circumference, should be less than 1.0 to indicate healthy fat distribution patterns.
Women should aim for a waist circumference of 80 centimeters or less, while men should target 90 centimeters or less, as excess abdominal fat is particularly associated with insulin resistance and diabetes complications.
Even modest weight loss representing just 5% of total body weight can produce significant improvements in blood sugar control, cholesterol levels, and blood pressure, making sustainable weight management goals both achievable and highly beneficial.
Medical Management
Medical intervention for diabetes varies significantly based on the type of diabetes diagnosed and individual patient factors that influence treatment effectiveness.
Personalized treatment plans are developed in collaboration between patients and their healthcare teams to address specific needs and circumstances.
For Type 1 Diabetes:
Type 1 diabetes management requires regular insulin administration as prescribed by healthcare providers, with dosing carefully calculated based on individual insulin sensitivity, carbohydrate intake, and activity levels.
Patients must master carbohydrate, fat, and protein counting to accurately match insulin doses with food consumption, ensuring optimal blood glucose control throughout the day.
Frequent blood sugar monitoring is essential for making real-time adjustments to insulin doses and detecting patterns that inform long-term management strategies.
Working closely with diabetes educators or registered dietitians provides patients with the knowledge and skills necessary to navigate complex daily management decisions and maintain long-term health.
For Type 2 Diabetes:
Treatment typically begins with diet and exercise modifications. If these alone are insufficient, medication may be necessary:
- Oral Medications: Various classes target different aspects of glucose regulation:
- Biguanides (e.g., Metformin/Glucophage®)
- Help the body use insulin more effectively and decrease liver glucose production
- Taken with meals to reduce stomach side effects
- May cause stomach discomfort, nausea, vomiting, diarrhea, loss of appetite, or metallic taste
- Sulphonylureas (e.g., Glipizide, Gliclazide, Glimepiride)
- Stimulate the pancreas to release more insulin
- Taken immediately before meals
- May cause weight gain
- Require consistent meal timing to prevent low blood sugar
- Dipeptidyl Peptidase-4 (DPP-4) Inhibitors (e.g., Linagliptin, Sitagliptin)
- Increase insulin release after meals and reduce liver glucose production
- Can be taken before or after food
- Monitor for signs of pancreatitis (severe stomach pain, nausea, vomiting)
- Sodium-Glucose Co-Transporter-2 (SGLT2) Inhibitors (e.g., Dapagliflozin, Empagliflozin)
- Prevent kidney reabsorption of glucose, increasing urinary glucose excretion
- May cause genital and urinary tract infections
- May cause low blood pressure and dizziness
- Maintain good genital hygiene when using these medications
- Alpha-Glucosidase Inhibitors (e.g., Acarbose/Glucobay®)
- Slow carbohydrate breakdown from food, reducing post-meal glucose spikes
- Taken immediately before or with the first mouthful of food
- May cause stomach discomfort, bloating, or diarrhea
- Meglitinides (e.g., Repaglinide/Novonorm®)
- Help the pancreas release more insulin
- Taken immediately before meals
- Require consistent meal timing
- Thiazolidinediones (e.g., Pioglitazone/Actos®)
- Make the body more sensitive to insulin
- Can be taken before or after food
- Inform healthcare providers about any heart conditions or fall history
- Biguanides (e.g., Metformin/Glucophage®)
- Insulin Therapy: May be required for some Type 2 diabetes patients, particularly in later stages of the disease.
Monitoring and Follow-up
Effective diabetes management requires ongoing monitoring:
- Regular Blood Glucose Monitoring
- Healthcare providers will advise patients on the appropriate frequency of blood glucose monitoring based on their individual treatment plan, diabetes type, and current level of glycemic control.
- This monitoring may involve using a traditional blood glucose meter at home, requiring finger stick blood samples several times daily to track glucose patterns and trends.
- Some patients, particularly those with Type 1 diabetes or those experiencing frequent glucose fluctuations, benefit significantly from continuous glucose monitoring systems that provide real-time glucose readings and trend information without the need for frequent finger sticks.
- Regular Medical Check-ups
- Scheduled medical appointments allow healthcare providers to monitor for potential diabetes complications such as cardiovascular disease, kidney problems, eye damage, and nerve dysfunction.
- These visits provide opportunities to adjust treatment plans as needed based on current blood glucose control, lifestyle changes, and emerging health concerns.
- Healthcare providers also screen for related conditions that commonly occur alongside diabetes, including high blood pressure, elevated cholesterol levels, and thyroid disorders, ensuring comprehensive health management.
- HbA1c Testing
- HbA1c testing is typically performed every 3-6 months and provides healthcare providers with an overview of average blood glucose levels over the past 2-3 months.
- This test is invaluable for assessing the effectiveness of current treatment strategies and making informed decisions about medication adjustments or lifestyle interventions.
Support and Resources in Singapore
Singapore’s healthcare system offers various support mechanisms for diabetes management:
- Subsidized Screening Programs
- The Screen for Life program offers subsidized diabetes screening for eligible individuals, making early detection and prevention more accessible to the general population.
- The Diabetes Risk Assessment (DRA) is a valuable tool that helps identify individuals at higher risk for developing diabetes, enabling early intervention and prevention strategies.
- Specialist Diabetes Care
- Singapore provides access to experienced endocrinologists and diabetes specialists at both public and private hospitals, ensuring patients receive expert medical care tailored to their specific needs.
- Diabetes nurse educators play a crucial role in providing comprehensive education and ongoing support, helping patients develop the skills and confidence necessary for successful self-management.
- Community Resources
- Various support groups and education programs are available throughout Singapore, providing patients with opportunities to connect with others facing similar challenges and learn from shared experiences.
- Healthy lifestyle promotion initiatives sponsored by government and community organizations help create supportive environments that encourage diabetes-friendly behaviors and choices.
Success Factors in Diabetes Management
Several factors contribute to successful diabetes management:
- Medication Adherence
- Taking medications exactly as prescribed by healthcare providers is fundamental to achieving optimal blood glucose control and preventing complications.
- Patients should understand that diabetes medications are not habit-forming and are essential tools for managing their condition effectively.
- It’s important to recognize that diabetes medications only work when taken consistently according to the prescribed schedule, making adherence a critical component of successful management.
- Self-monitoring
- Regular blood glucose checking enables patients to understand how their body responds to different foods, activities, medications, and stressors throughout the day.
- Recognizing patterns and triggers helps patients make informed decisions about their daily management strategies and identify areas where adjustments may be needed.
- Taking appropriate action when glucose levels fall outside the target range, whether through medication adjustment, dietary changes, or activity modification, empowers patients to maintain better overall control of their condition.
- Education
- Developing a thorough understanding of diabetes and its management principles enables patients to make informed decisions about their daily care and long-term health strategies.
- Recognizing early signs of complications such as cardiovascular problems, kidney disease, or nerve damage allows for prompt medical intervention and better outcomes.
- Knowing when to seek medical help, whether for routine care or urgent situations, ensures patients receive appropriate care when needed and avoid potentially serious complications.
- Support Network
- Active involvement of family and friends in diabetes management provides emotional support and practical assistance that can significantly improve adherence to treatment plans and overall quality of life.
- Effective collaboration with the healthcare team, including physicians, nurses, dietitians, and other specialists, ensures comprehensive care that addresses all aspects of diabetes management.
- Utilizing community resources such as support groups, educational programs, and wellness initiatives provides additional layers of support and motivation that contribute to long-term success in diabetes management.
FAQ Section
What is diabetes mellitus?
Diabetes mellitus is a chronic metabolic condition characterized by elevated blood glucose levels resulting from the body’s inability to produce sufficient insulin or use insulin effectively.
Insulin is essential for transferring glucose from the bloodstream into cells for energy.
When this process is impaired, blood sugar levels rise, leading to various health complications if not properly managed.
How common is diabetes in Singapore?
Diabetes affects approximately 1 in 10 Singaporeans, with prevalence increasing to about 1 in 3 among those over 60 years old.
The Ministry of Health estimates that roughly one-third of people with diabetes in Singapore are unaware of their condition, highlighting the importance of regular screening.
What are the main types of diabetes?
There are three main types of diabetes. Type 1 diabetes is an autoimmune condition where the pancreas produces little or no insulin, typically developing rapidly and often at younger ages.
Type 2 diabetes occurs when the body becomes resistant to insulin or doesn’t produce enough insulin, developing gradually and more commonly in adults with risk factors such as obesity and sedentary lifestyle.
Gestational diabetes appears during pregnancy and usually resolves after childbirth, though it increases future diabetes risk.
What are the risk factors for developing diabetes?
Key risk factors include age (especially over 45), overweight or obesity (BMI ≥23), family history of diabetes, physical inactivity, history of gestational diabetes, polycystic ovary syndrome, and certain ethnicities.
In Singapore, those of Indian and Malay descent tend to have higher prevalence rates than those of Chinese descent.
How is diabetes diagnosed in Singapore?
Diabetes diagnosis in Singapore typically involves one or more blood tests: fasting blood glucose test (after 8+ hours fasting), casual blood glucose test (random testing), HbA1c test (measuring average blood glucose over 2-3 months), or oral glucose tolerance test (measuring how quickly glucose is cleared from the blood). Diagnosis is based on established thresholds for each test.
What lifestyle changes help manage diabetes?
Effective lifestyle management includes maintaining a balanced diet low in refined carbohydrates, saturated fats, and added sugars while rich in fiber, lean proteins, and healthy fats. Regular physical activity (at least 150 minutes weekly of moderate exercise) is crucial. Weight management, stress reduction, adequate sleep, and avoiding tobacco and excessive alcohol also significantly improve diabetes control.
What medications are used to treat diabetes in Singapore?
Treatment may include oral medications like Metformin (improves insulin sensitivity), Sulphonylureas (increase insulin production), DPP-4 inhibitors (enhance post-meal insulin release), SGLT2 inhibitors (increase glucose excretion), and others. Insulin therapy is essential for Type 1 diabetes and may be needed for some with Type 2 diabetes. The specific medication regimen depends on individual factors, diabetes type, and control levels.
How often should someone with diabetes get checked?
People with diabetes should typically have HbA1c levels checked every 3-6 months, with more frequent monitoring for those with unstable blood glucose or recent medication changes. Annual comprehensive examinations should include eye, kidney, nerve, and cardiovascular assessments. Self-monitoring frequency varies by individual needs, medication regimen, and physician recommendations.
Will I become dependent on diabetes medications?
No, you cannot become dependent on diabetes medications in the way one might become dependent on addictive substances.
Diabetes medications help manage blood glucose levels when taken as prescribed but don’t create physical dependency.
However, your body continues to need these medications to maintain proper glucose control.
Some people with Type 2 diabetes may reduce or eliminate medication needs through significant lifestyle changes and weight loss, but this should only be done under medical supervision.
How does exercise help in managing diabetes?
Exercise improves diabetes management by increasing insulin sensitivity, allowing cells to absorb glucose more efficiently with less insulin. During physical activity, muscles can absorb glucose without insulin.
Regular exercise lowers blood glucose levels, reduces HbA1c, improves cardiovascular health, helps with weight management, reduces stress, and enhances overall well-being.
Both aerobic exercise and resistance training provide benefits, with recommendations for at least 150 minutes of moderate activity weekly, spread across several days.
What subsidies are available for diabetes care in Singapore?
Singapore offers several subsidy programs for diabetes care. The Screen for Life program provides subsidized screening for Singapore citizens and Permanent Residents aged 40 and above.
MediSave can be used for outpatient treatment of chronic conditions including diabetes under the Chronic Disease Management Programme.
The Community Health Assist Scheme (CHAS) offers subsidies at participating clinics for lower and middle-income households.
Additional support may be available through hospital-based medical social workers for those facing financial difficulties.
Can diabetes be cured?
Type 1 diabetes currently has no cure and requires lifelong insulin therapy. For Type 2 diabetes, while it cannot be “cured” in the traditional sense, some people can achieve remission through significant lifestyle changes, particularly substantial weight loss.
Remission means maintaining normal blood glucose levels without medication, but the underlying condition remains, requiring continued monitoring and healthy lifestyle maintenance.
Bariatric surgery has shown promising results for some people with Type 2 diabetes and obesity, potentially leading to long-term remission.
What complications can arise from poorly managed diabetes?
Poorly managed diabetes can lead to numerous complications affecting various body systems. Cardiovascular complications include heart disease, stroke, and peripheral arterial disease.
Microvascular complications affect small blood vessels, leading to kidney disease (nephropathy), eye damage (retinopathy), and nerve damage (neuropathy).
Additional complications may include foot problems potentially requiring amputation, skin conditions, hearing impairment, Alzheimer’s disease, and depression.
Maintaining good glucose control significantly reduces these risks.
How do I know if my diabetes is well-controlled?
Well-controlled diabetes is typically indicated by HbA1c levels below 7% (or individualized targets set by your healthcare provider), fasting blood glucose between 4-7 mmol/L, and post-meal readings below 10 mmol/L.
Beyond these numbers, consistent readings within your target range, minimal episodes of hypoglycemia (low blood sugar), stable weight, good energy levels, and absence of diabetes symptoms also suggest good control.
Regular monitoring and follow-ups with healthcare providers help evaluate overall management effectiveness.
What should I do during sick days if I have diabetes?
During illness, continue taking diabetes medications unless otherwise advised by your healthcare provider. Monitor blood glucose more frequently (every 2-4 hours) as illness often raises levels.
Stay hydrated with sugar-free fluids and maintain nutrition with easily digestible foods if possible.
Have a clear sick-day plan developed with your healthcare team, including when to seek medical attention (persistent vomiting, difficulty breathing, very high or low blood glucose, or symptoms of diabetic ketoacidosis).
Contact your healthcare provider if illness persists beyond a couple of days.

