Understanding Migraines: More Than Just Headaches
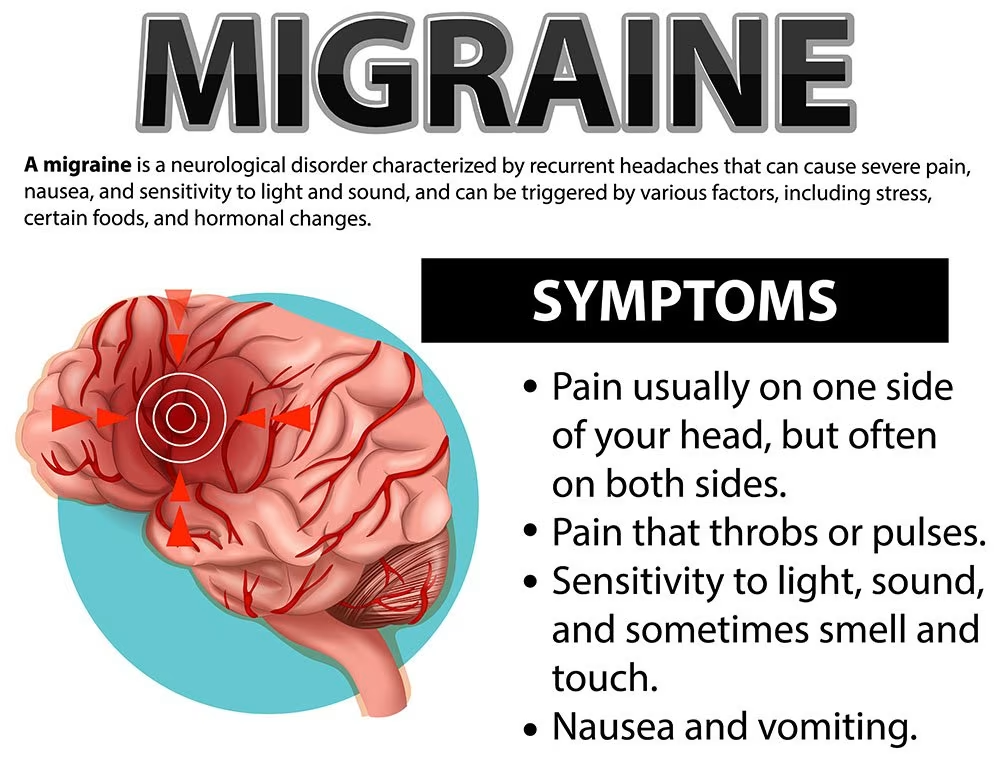
Migraines are far more than ordinary headaches. They can be extremely debilitating, and when a migraine attack occurs, sufferers usually have difficulty resuming normal activities and often have to retreat to bed to ride it out.
A migraine is a very painful type of headache that usually begins slowly, worsens over minutes to hours, and resolves slowly at the end of an attack.
The pain is typically a moderate or severe throbbing sensation that worsens with movement and prevents normal activities.
In addition to severe throbbing pain on one or both sides of the head, migraine sufferers may also experience nausea, vomiting, dizziness, visual auras (flashing colorful lights, lines or shadows) and tingling in the face, hands or feet.
Many are extremely sensitive to sound, touch, smells and bright lights during an attack.
The constant stress of wondering when the next attack may occur and the lack of understanding from colleagues and loved ones can also take a toll. Migraineurs are also more likely to suffer from depression.
Related article: Health Screening in Singapore
Prevalence in Singapore
In Singapore, migraine affects around 330,000 people, and that number continues to grow. According to a 2018 Singapore study, the direct and indirect costs due to migraines were estimated to be S$1.04 billion.
Migraines are common in Singapore, with a lifetime prevalence of 8.2% in a recent 2020 study. The prevalence is similar between boys and girls before puberty, at around 3-7%.
However, after puberty, due to hormonal influences, migraines become three times more common in females than males, continuing until menopause when there’s a decline.
In the 2020 Singapore study, certain demographic groups were more likely to experience migraine headaches:
- Malay ethnicity (compared to Chinese)
- Diploma holders (compared to degree holders)
- Younger adults aged 18-34 years (compared to those 65 years and above)
- Employed people (compared to economically inactive people)
You might like: Best JB Health Screening Clinics for Singaporeans
Types of Migraines
By international classification criteria, migraines can be subdivided into episodic migraines and chronic migraines:
- Patients with episodic migraines experience migraines at a frequency of four to 14 days a month, over a period of at least three months.
- Patients with chronic migraines have headache days occurring at more than 15 days a month over a period of three months.
Chronic migraines represent a more severe form, with neurophysiology studies and functional neuroimaging showing brain changes that are different from patients with episodic migraines or those without migraines. As such, treatment approaches differ between these two types.
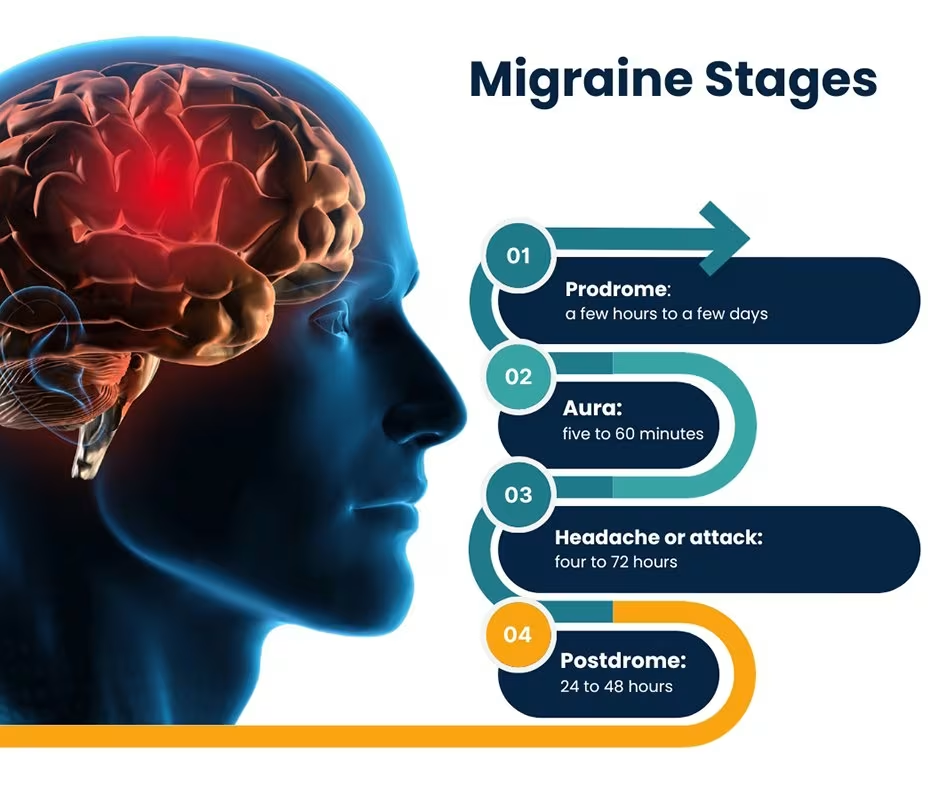
Some people experience what’s known as “Silent Migraine,” where they may have migraine symptoms without the actual headache. For others, migraines progress through several distinct phases:
The Phases of Migraine
- The Prodromal Phase: In the early stages, one or two days before a migraine, pre-migraine warning signs may appear. These can include: constipation, depression, food cravings, hyperactivity, irritability, neck stiffness, and in some cases, uncontrollable yawning.
- The Aura Phase: About one in five people experiences nervous system symptoms such as visual disturbances. A typical visual aura presents as a flickering, jagged or zigzag line that seems to appear at the corner of one’s vision. Another sign is numbness and tingling of the lips, lower face and fingers of one hand. Some people may experience temporary paralysis on one side of the body.
This might help: Best Chiropractor in Singapore (Sort by Reviews)
Auras rarely last longer than an hour and in most cases, are followed by a headache. Some people do not experience the aura phase, but may have symptoms such as mood changes, fatigue, mental fuzziness, fluid retention, diarrhea, increased urination, nausea and vomiting.
- The Attack Phase: The migraine attack itself can last for a few hours to several days. The throbbing pain usually begins above the eyes and affects one side of the head. The pain may affect the entire head or move from one side to the other or spread to the lower face and the neck. It worsens during physical activity.
- The Postdromal Phase: In the aftermath of a migraine episode, the sufferer may feel extremely euphoric.
Related article: Anxiety Therapy in Singapore: Treatment and Recovery
Diagnosing Migraines in Singapore
The mean age of onset of migraines in Singapore is 26.4 years, with a bimodal distribution of peaks in the late teens and twenties and around 50 years of age.
However, patients with migraines can present at any age, and a careful history taking is needed to differentiate primary headache disorders, such as migraines and tension-type headaches, from secondary headache disorders.
If you have experienced migraines before but they have increased in severity or frequency, or if the attack is severe and comes on suddenly, like a “clap of thunder,” it’s important to consult a doctor.
Depending on the findings, your doctor may recommend further investigation including:
- Blood tests to test for blood vessel problems and infections
- Computerized tomography (CT) scan or Magnetic resonance imaging (MRI) to create detailed cross-sectional images of the brain
- Spinal tap (lumbar puncture) for suspected infections or bleeding in the brain
Migraine is a complicated condition and symptoms may not always be the same for everyone. They usually occur in a recognizable pattern and can generally be diagnosed easily. While migraine is treatable and not life-threatening, severe and frequent attacks can result in poor quality of life. If it becomes chronic, it can be difficult to eradicate.
This might help: Complete Guide to Depression Therapy in Singapore
Common Migraine Triggers
Identifying and avoiding triggers is crucial in managing migraines. Each migraine sufferer has their own individual triggers, so keeping a journal to track activities and events during a migraine attack will help identify specific triggers.
Over time, avoiding these triggers can reduce the number of attacks. Free smartphone apps such as “migraine buddy” can help track the condition.
Common triggers include:
- Lack of sleep
- Caffeine
- Stress
- Changes in hormones during menstrual cycle, pregnancy and menopause
- Alcohol
- Skipping meals
- Birth control pills
- Changes in temperature, humidity and barometric pressure
In addition to the diagnostic criteria, headaches with a clear trigger such as alcoholic beverages, menstruation, sleep deprivation, stress, missed meals, dehydration and other commonly known migraine triggers also give clues to the diagnosis of migraines.
You might like: Alcohol Addiction Treatment in Singapore
According to studies, the most common migraine triggers and their prevalence include:
| Migraine Trigger | Percentage (%) |
|---|---|
| Stress | 79.7 |
| Hormones | 65.1 |
| Missing a meal/hunger/fasting | 57.3 |
| Weather change | 53.2 |
| Sleep disturbance | 49.8 |
| Perfume or odour | 43.7 |
| Neck pain | 38.4 |
| Light | 38.1 |
| Alcohol | 37.8 |
| Smoking | 35.7 |
| Sleeping late | 32.0 |
| Heat | 30.3 |
| Food | 26.9 |
| Exercise | 22.1 |
| Sexual activity | 5.1 |
Treatment Approaches for Migraines in Singapore
Once migraine has been diagnosed, your doctor can determine treatments that can help stop symptoms and prevent future attacks. These fall into 2 broad categories:
- Pain-relieving medications designed to stop symptoms once an attack begins.
- Preventive medications usually prescribed for chronic migraine and taken regularly, often on a daily basis, to reduce the severity or frequency of attacks.
Non-Pharmacological Management
For the non-pharmacological approach, trigger identification and lifestyle modification play significant roles in limiting the progression and chronification of migraines.
A healthy lifestyle with avoidance of triggers allows for less frequent attacks, hence minimizing the risk of developing higher frequency or chronic migraines.
Other than using medications to treat the condition, migraine can also be managed by the following methods:
- Drink water to avoid dehydration, especially if you are vomiting
- Rest in a dark, quiet room
- Place a piece of cool cloth on your head
The following are some suggestions to prevent migraines from happening again:
- Avoid foods and situations that cause your migraines
- Avoid smoking
- Avoid alcohol
- Get plenty of sleep each night
- Learn to relax and reduce stress
Related article: Complete Guide to Anger Management in Singapore
Pharmacological Management
Acute Symptomatic Treatment
Adequate abortive treatment is needed to ensure a good quality of life for the patient. Physicians can consider acute pain management of migraines using either a step-care approach or a stratified-care approach.
In a step-care approach, patients are given first-line abortive treatments such as acetaminophen before escalating to nonsteroidal anti-inflammatory drugs (NSAIDs) or triptans should the first-line medications fail.
For a stratified-care regimen, physicians can use assessment tools to evaluate severity and disability from migraine attacks, and therefore be better able to predict analgesia needs.
A low score indicates that the patient is less likely to require escalation of treatment and can be started on acetaminophen or NSAIDs first. Patients with a higher score may respond better to migraine-specific treatments such as triptans as first-line therapy.
Available medications for acute treatment include:
- Paracetamol, Paracetamol with Codeine, Paracetamol with Codeine and Caffeine
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs) such as Ibuprofen, Naproxen, Diclofenac
Preventive Treatment
The choice to start preventive treatment requires proper discussion between the physician and patient.
While it is common to start preventive treatment for patients with high-frequency episodic migraines or chronic migraines, preventive treatment can also be considered for low-frequency episodic migraine patients if each attack is severe, prolonged and debilitating.
The discussion needs to be based on the benefit of preventive treatment versus the harm from its side effects.
The choice of preventive is largely dependent on the patient’s comorbidities, ease of administration and side effects.
Preventive medications may include:
- Anti-depressants and anti-seizure medications even if you aren’t suffering from these conditions as such drugs have been seen to keep migraines at bay
- Botox injections
- Erenumab, a newer type of drug that blocks the action of CGRP, a molecule known to play a role in migraines
This might help: Complete Guide to Depression Therapy in Singapore
Your doctor will work with you to find out what medication is right for you so you can:
- Avoid potential side effects
- Ensure that what you are taking actually manages the pain
- Manage your tolerance for the medications prescribed on an ongoing basis
It’s important to note that dependence on migraine medications can actually cause headaches from overuse.
This might help: Anxiety Therapy in Singapore: Treatment and Recovery
Commonly Used Preventive Medications
| Drug | Starting dose | Key considerations |
|---|---|---|
| Propranolol | 10 mg BD | Benefits: Helps with hypertension<br>Side effects: Lethargy, nausea, postural giddiness<br>Avoid if: Asthma, depression, heart failure |
| Amitriptyline/Nortriptyline | 5-10 mg ON / 10 mg ON | Benefits: Helps with insomnia, depression, anxiety<br>Side effects: Drowsiness, dry mouth, weight gain<br>Avoid if: Urinary retention, heart blocks |
| Flunarizine | 5 mg ON | Benefits: Helps with hypertension<br>Side effects: Drowsiness, parkinsonism, weight gain<br>Avoid if: Parkinson disease, depression |
| Topiramate | 25 mg ON | Benefits: Helps with epilepsy, obesity<br>Side effects: Paresthesia, altered taste, cognitive issues<br>Avoid if: Renal stones, glaucoma |
| Valproate | 200-500 mg BD | Benefits: Helps with epilepsy, depression<br>Side effects: Weight gain, tremors, lethargy<br>Avoid if: Liver disease, thrombocytopenia |
When to See a Specialist
If your symptoms aren’t well controlled using the medications prescribed by your primary care doctor, you may be referred to various specialists depending on the types of symptoms you experience.
A neurologist specially trained in treating headaches, including migraines, can provide advanced care for complex cases.
An ophthalmologist may be recommended if you experience temporary blindness during your migraine attacks.
If your migraines are triggered mostly by stress, you might benefit from seeing a psychologist or psychiatrist.
An ear, nose, and throat (ENT) specialist can help if you experience sinus symptoms alongside your migraines. For hormone-related triggers, an obstetrician/gynecologist (OB/GYN) may be appropriate.
If you have access to one and your migraines are very severe, a pain-management specialist or migraine clinic can provide comprehensive care, often offering access to multiple specialists in one location.
When to Seek Emergency Medical Attention
Don’t wait to seek help if you experience any of the following warning signs. Seek immediate medical attention if you have a “thunderclap” headache, can’t stop vomiting, lose part of your sight during a migraine, experience a headache that lasts more than 72 hours, or develop any new symptoms.
Consult a doctor immediately or go to the emergency department if your headache is abrupt and severe, occurs with a fever, happens after a head injury (especially if it gets worse), or lasts for days or weeks and worsens after coughing, exertion, straining, or sudden movement.
Tracking Your Migraines
Because migraines can have many triggers, keeping a diary can help you and your doctor identify specific patterns.
Take note of the day and time the pain started, what you ate and drank over the last 24 hours, and the amount of sleep you had the previous night.
Record what you were doing and where you were before the pain started, how long the headache lasted, and what helped to ease it.
Related Medical Conditions
Many people who suffer from migraines also experience various other health issues that commonly coexist with migraine, though the causes aren’t always clear.
Depression and anxiety frequently coexist in many migraine sufferers. Cardiovascular disease presents a slightly increased incidence among those with migraines.
Nasal or sinus inflammation conditions affect many migraine sufferers as well. Certain medications can create headache patterns that become migraine-like.
Additionally, trauma or hemorrhages to the brain from head or neck injuries, as well as infections, may be related factors.
Evaluating a patient’s family history for headache conditions allows healthcare providers to identify familial patterns and genetic predisposition to migraines.
Migraines commonly occur among first-degree relatives, with studies showing that a strong family history predisposes individuals to earlier onset, higher numbers of medication days, and more severe symptoms.
FAQ
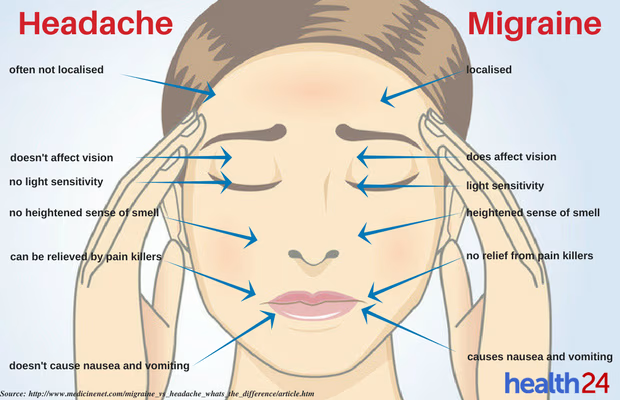
What is the difference between a migraine and a regular headache?
A migraine is not just a headache but a chronic and more localized condition. While a common headache like a tension headache is associated with stress or fatigue and causes continuous but not throbbing pain, migraines cause severe throbbing pain on one or both sides of the head, often accompanied by nausea, vomiting, and sensitivity to light and sound. Migraines typically progress through several stages and can be much more debilitating.
How common are migraines in Singapore?
Migraines are common in Singapore, with a lifetime prevalence of 8.2% according to a recent 2020 study. The condition affects around 330,000 people in Singapore, and that number continues to grow.
What are the warning signs of an impending migraine?
You may experience warning signs just before a migraine develops. These early indicators can include feeling very tired and yawning frequently, craving certain foods or feeling unusually thirsty, experiencing changes in your mood, or developing a stiff neck.
You may also experience specific warning signs known as an “aura” that indicate you’re about to have a migraine.
These aura symptoms can include problems with your vision, such as seeing zigzag lines, bright spots, or flashing lights.
You might experience numbness or tingling in the fingers of one hand, lips, tongue, or lower face.
Feeling dizzy or having difficulty speaking are also common aura symptoms.
When should I see a doctor about my migraines?
Although migraines can often be treated without a doctor’s consultation, there are times when the condition might be more serious and require medical attention.
You should see a doctor if your condition does not improve within three days, if aura symptoms last longer than an hour at a time, or if symptoms worsen.
You should also seek medical care if you experience speech, vision, or movement problems, or if you lose your balance.
Additional concerning signs include headaches that are worse when lying down, treatments that once worked but are no longer helpful, changes in headache patterns or pain characteristics, or headaches that start very suddenly.
What medications are used to treat migraines in Singapore?
Migraines can be treated with various medications that you can obtain from your pharmacist. Over-the-counter options include paracetamol, paracetamol with codeine, and paracetamol with codeine and caffeine.
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, and diclofenac are also effective treatment options.
For preventive treatment, your doctor may prescribe anti-depressants and anti-seizure medications, even if you aren’t suffering from depression or seizures.
Botox injections may be recommended for certain cases. Erenumab, a newer type of drug that blocks the action of CGRP (a molecule known to play a role in migraines), represents an advanced treatment option.
How can I prevent migraine attacks?
To prevent migraines from recurring, you should avoid foods and situations that trigger your migraines.
Lifestyle modifications include avoiding smoking and alcohol, ensuring you get plenty of sleep each night, and learning to relax and reduce stress.
Keeping a journal to track activities and events during a migraine attack will help identify your personal triggers.
There are also free smartphone apps such as “migraine buddy” that can help you keep track of your condition.
What is chronic migraine and how is it different from episodic migraine?
Most people who suffer migraines have episodic migraines that last for a few hours and happen every now and again, or at most once or twice a month. The unlucky 2% of the world’s population with chronic migraine suffers from headaches at least 15 days a month and the attacks tend to last longer. This makes living a normal life very challenging.
Chronic migraines represent a more severe form of migraine, with neurophysiology studies and functional neuroimaging showing changes in the brain that are different from patients with episodic migraines or patients without migraines. As such, treatment approaches differ between these types.
Can hormones affect migraines?
Due to the influence of hormones, the prevalence of migraines becomes higher in females after puberty, with migraines being three times more common than in males.
This higher prevalence amongst females continues until menopause with a decline in statistics thereafter, but remains slightly higher than in males.
Migraines can happen to anyone, but they tend to be more common in adult women than men.
Some women may find that migraine attacks tend to coincide with hormonal changes and occur just before or shortly after onset of menstruation.
What should I do during a migraine attack?
During a migraine attack, these methods can help manage the condition:
- Drink water to avoid dehydration, especially if you are vomiting
- Rest in a dark, quiet room
- Place a piece of cool cloth on your head
For medication, you can approach your pharmacist for Paracetamol (with or without Codeine and Caffeine) or Non-Steroidal Anti-inflammatory Drugs (NSAIDs) such as Ibuprofen, Naproxen, or Diclofenac.
Are there any new treatments for migraines available in Singapore?
Erenumab, a new type of drug that blocks the action of CGRP (a molecule known to play a role in migraines), is one of the newer treatments available. Botox injections are also used as a preventive treatment for chronic migraines.
How are migraines related to other health conditions?
Many people who suffer from migraines also suffer from other health issues that commonly coexist with migraine.
These include depression and anxiety, cardiovascular disease, nasal or sinus inflammation conditions, and certain medications which can create a headache pattern that becomes migraine-like.
Trauma or hemorrhages to the brain from head or neck injury, and infections can also be related to migraines.
By understanding the nature of migraines, identifying personal triggers, and working with healthcare professionals in Singapore, it’s possible to effectively manage this condition and improve quality of life.
While there’s no permanent cure for migraines, a combination of preventive strategies and appropriate treatments can significantly reduce their frequency and severity.

