Understanding Eczema: Causes, Types, and Symptoms
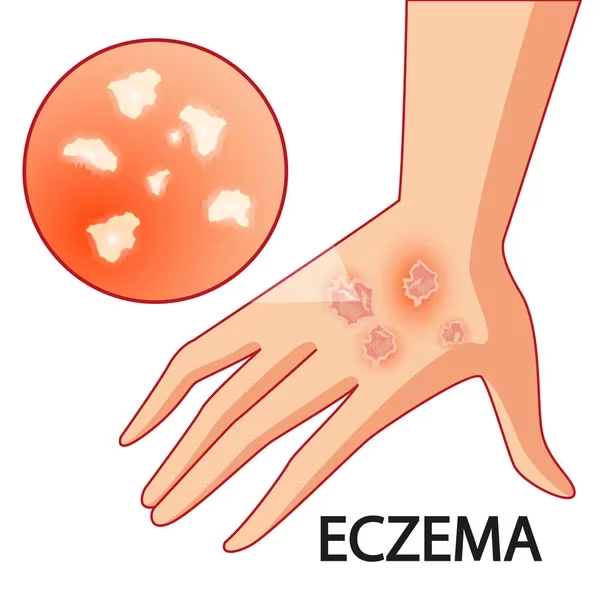
Eczema, also known as dermatitis, is a common skin condition that causes the skin to become inflamed, itchy, and red.
The term “eczema” comes from the Greek word meaning “to boil over,” aptly describing how the skin appears during flare-ups.
While “dermatitis” refers to skin inflammation, “atopic” pertains to an allergic tendency, which is why the most common form is called atopic dermatitis.
In Singapore, eczema is particularly prevalent, affecting up to 20% of school children and a significant number of adults. Reports indicate that at least one in ten Singaporean adults suffers from eczema, with approximately eight new cases reported daily.
Read more: Guide to Seeing a Dermatologist in Singapore
What Causes Eczema?
While the exact cause of eczema remains unknown, several factors contribute to its development:
- Genetic factors: People with a family history of eczema, asthma, or allergic rhinitis have a higher likelihood of developing eczema.
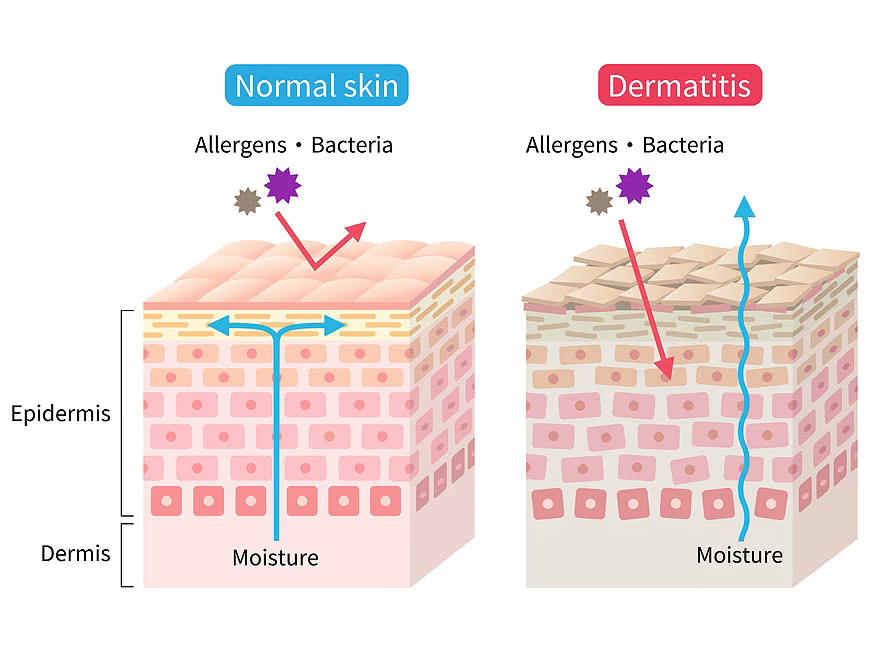
- Skin barrier dysfunction: Individuals with eczema typically have a thinner lipid barrier in their skin, leading to increased water loss and dry skin.
- Immune system issues: An overactive immune system responds aggressively to irritants on the skin by releasing inflammatory chemicals beneath the skin surface.
- Environmental triggers: Various external factors can trigger or worsen eczema flare-ups.
Common Eczema Triggers
Eczema flare-ups can be triggered by a wide variety of environmental and lifestyle factors that individuals should be aware of to better manage their condition.
Changes in climate, particularly extreme heat or cold conditions and exposure to haze, can significantly irritate sensitive skin and precipitate eczema symptoms.
Environmental allergens such as dust mites and dusty environments are common triggers that affect many eczema sufferers, especially in indoor settings with poor air circulation.
Excessive sweating from physical activity or hot weather can irritate the skin and worsen eczema symptoms, while exposure to cigarette smoke, whether from personal smoking or secondhand exposure, can trigger inflammatory responses.
Strong soaps, detergents, and bubble baths containing harsh chemicals can strip the skin’s natural protective barrier and cause irritation in sensitive individuals.
Related article: Which Dermatologist in Singapore Should You Consider? (Sort by Reviews)
Contact with synthetic materials or wool clothing can cause mechanical irritation and trigger eczema flare-ups due to the rough texture and potential chemical treatments in these fabrics.
Common household items such as pets, carpets, and stuffed toys can harbor allergens and dust mites that contribute to eczema symptoms in susceptible individuals.
Respiratory infections including flu and upper respiratory tract infections can trigger eczema through immune system activation, while skin infections caused by bacterial, viral, or fungal organisms can worsen existing eczema or trigger new outbreaks.
Insect bites can cause localized inflammation that may spread and trigger broader eczema symptoms in sensitive individuals.
Psychological stress is a well-recognized trigger that can worsen eczema through various biological pathways, while scratching creates a destructive itch-scratch cycle that perpetuates and worsens symptoms.
Even beneficial medical interventions such as vaccinations can temporarily trigger eczema, though these should never be avoided—patients should simply moisturize their skin regularly during the vaccination period.
Food allergies contribute to eczema in approximately 10-15% of cases, with this association being particularly common in young children.
You might like: Best Dermatologist in JB for Singaporeans
Types of Eczema and Their Symptoms
Atopic Dermatitis
This is the most common form of eczema, typically starting in childhood but can also develop in adulthood. It often co-occurs with asthma and hay fever (the “atopic triad“).
- The characteristic symptoms of atopic dermatitis include distinctive rashes that develop in the creases of elbows or knees, creating a typical distribution pattern that helps with diagnosis.
- Over time, the skin in affected areas may become lighter, darker, or significantly thicker compared to surrounding normal skin, reflecting chronic inflammation and repeated scratching.
- Small bumps frequently develop that leak fluid when scratched, creating weeping lesions that can become infected if not properly managed.
- In babies and infants, rashes typically appear on the scalp and cheeks rather than in body creases, representing a different distribution pattern compared to older children and adults.
Causes include:
- The constant urge to scratch significantly increases the risk of secondary bacterial infections, which can complicate treatment and prolong healing times.
You might like: A Complete Guide To Laser And Skin Treatments In Singapore
Contact Dermatitis
This occurs due to contact with irritants or allergens and comes in two types: allergic contact dermatitis (immune system reaction) and irritant contact dermatitis (damaged skin cells without allergic reaction).
Symptoms include:
- Both forms of contact dermatitis produce similar symptoms, including intense itchiness accompanied by redness and stinging sensations that can range from mild to severe.
- Patients often develop itchy bumps or hives in the affected areas, along with fluid-filled blisters that may ooze clear or yellowish fluid and subsequently become crusty as they heal.
- Over time, affected skin becomes thickened and scaly due to chronic inflammation and repeated exposure to triggering substances.
Causes include:
- Irritant contact dermatitis commonly results from exposure to harsh detergents, bleach, poison ivy, or tobacco smoke, while allergic contact dermatitis is frequently triggered by nickel found in jewelry and buckles, latex products, fragrances in cosmetics and cleaning products, or makeup containing sensitizing ingredients.
You might like: What Treatment is Best for Anti-Aging?
Dyshidrotic Eczema (Hand and Feet Eczema)
Dyshidrotic eczema specifically affects the hands and feet and is characterized by the development of small, intensely itchy blisters. This condition shows a higher prevalence in women compared to men, though it can affect individuals of any gender.
Symptoms include:
- The primary symptoms include fluid-filled blisters that develop on fingers, toes, palms, and soles, creating distinctive clusters that can be both visually striking and functionally impairing.
- These blisters typically cause significant itchiness or pain that can interfere with daily activities and sleep patterns.
- As the condition progresses, affected skin undergoes scaling, cracking, and flaking, which can create open wounds susceptible to secondary infections.
Causes include:
- Several factors can contribute to dyshidrotic eczema development, including underlying allergies to environmental or contact substances, prolonged exposure to damp conditions that keep hands and feet moist, direct exposure to metals such as nickel, cobalt, or chromium salt commonly found in jewelry and industrial products, and psychological stress that can trigger or worsen symptoms.
Related article: Melasma Treatment in Singapore
Hand Eczema
Hand eczema specifically affects only the hands and represents a significant occupational health concern for individuals whose work involves frequent contact with irritating substances or requires repeated hand washing and chemical exposure.
Symptoms include:
- The condition manifests as red, itchy, and persistently dry hands that may feel tight and uncomfortable throughout the day.
- Affected individuals frequently develop painful cracks and fluid-filled blisters on their hands, which can significantly impair hand function and make routine tasks difficult or impossible to perform.
Common occupational triggers:
- Common occupational triggers include cleaning work that involves repeated exposure to detergents and disinfectants, hairdressing activities that require contact with hair chemicals and frequent hand washing, healthcare work involving repeated hand sanitizing and glove use, and laundry or dry cleaning operations that expose workers to various cleaning chemicals and solvents.
You might like: Guide to Wart Removal in Singapore
Neurodermatitis
Neurodermatitis shares similarities with atopic dermatitis but typically develops in individuals who already have other types of eczema or psoriasis, representing a complication of existing skin conditions rather than a primary disorder.
Symptoms include:
- This condition is characterized by thick, scaly patches that can develop on various body parts including arms, legs, neck, scalp, feet, hands, and genital areas.
- The patches often have a leathery appearance due to chronic scratching and inflammation.
- One of the most challenging aspects of neurodermatitis is the intense itching that typically worsens when patients are sleeping or relaxing, disrupting sleep patterns and quality of life.
Common occupational triggers:
- The persistent scratching associated with this condition creates a significant risk of bleeding and secondary bacterial infections, which can complicate treatment and potentially lead to scarring or permanent skin changes.
Nummular Eczema
Nummular eczema is characterized by distinctive round, coin-shaped spots on the skin, with the term “nummular” derived from the Latin word meaning “coin,” which accurately describes the appearance of these lesions.
Symptoms include:
- The condition presents as round, coin-shaped spots that are clearly demarcated from surrounding normal skin.
- These spots typically cause significant itchiness and may develop scaling or crusting as they progress through different stages of inflammation.
Causes include:
- Several factors can contribute to nummular eczema development, including insect bites that trigger localized inflammatory responses, allergic reactions to metals such as nickel or chromium or chemicals found in personal care products, underlying dry skin conditions that compromise the skin barrier, and having other pre-existing forms of eczema that predispose individuals to developing this variant.
Stasis Dermatitis
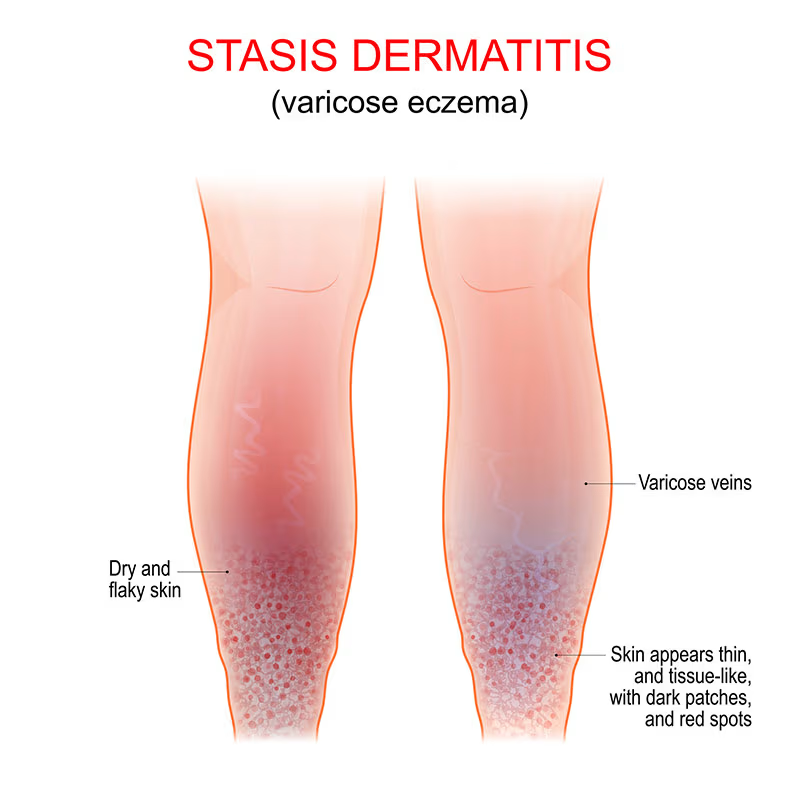
Stasis dermatitis develops when fluid leaks from weakened veins into surrounding skin tissues, making it particularly common in individuals with poor circulation, especially affecting the lower extremities.
As stasis dermatitis progresses, patients develop dryness and intense itchiness of the skin above the varicose veins, which can lead to scratching and further skin damage.
In advanced cases, open sores may develop on the lower legs and tops of feet, creating chronic wounds that heal slowly and are prone to infection.
Symptoms include:
- The condition typically begins with swelling of the lower legs that may worsen throughout the day and improve with elevation.
- Patients frequently experience aching or heaviness in their legs, particularly after prolonged standing or walking.
- Varicose veins are commonly visible and represent the underlying vascular problem causing the condition.
Related article: Vein Removal Treatment
Seborrheic Dermatitis
Seborrheic dermatitis specifically affects areas of the body with abundant oil-producing glands, most commonly involving the scalp where it manifests as dandruff, as well as the eyebrows, sides of the nose, and central chest areas.
Symptoms include:
- The condition is characterized by scaly, itchy patches that can range from mild flaking to thick, adherent scales.
- Affected areas typically show redness and inflammation that can be both cosmetically concerning and physically uncomfortable.
- In infants, seborrheic dermatitis may appear as “cradle cap,” presenting as thick, yellowish scales on the scalp that are generally harmless but may cause parental concern about the infant’s appearance and comfort.
Diagnosis of Eczema
Typically, a physical examination and medical history review are sufficient for a dermatologist to diagnose eczema. Laboratory tests are usually not necessary but may be ordered to:
- Rule out other skin conditions
- Identify potential allergic triggers
- Check for signs of infection
Common diagnostic methods include:
- Blood tests to check for elevated eosinophils or IgE antibody levels
- Patch testing to identify contact allergies
- Skin prick tests to identify allergic reactions
- Skin biopsy in some cases to rule out other skin diseases
Treatment Options for Eczema in Singapore
While there is no cure for eczema, various treatments can help manage symptoms and improve quality of life. The approach depends on the severity of the condition, age of the patient, and type of eczema.
Topical Treatments
1. Moisturizers (Emollients)
Moisturizers serve as the cornerstone of eczema management and are essential for maintaining optimal skin hydration and preventing inflammatory flare-ups.
These products should be applied liberally at least twice daily to maintain the skin’s protective barrier and prevent excessive dryness that can trigger eczema symptoms.
Fragrance-free creams or ointments are strongly preferable to lotions because they provide superior hydration and are less likely to contain irritating additives that can worsen sensitive skin conditions.
For maximum effectiveness, moisturizers should be applied within five minutes after bathing while the skin is still damp, as this timing helps lock in moisture and enhances the product’s hydrating benefits.
This practice, known as the “soak and seal” method, significantly improves skin barrier function and reduces the frequency of eczema flare-ups.
2. Topical Corticosteroids
Topical corticosteroids represent the primary treatment approach for managing inflammation and itching associated with eczema flare-ups.
The strength of these medications varies significantly based on the patient’s age, the severity of symptoms, and the specific body area being treated, with more potent formulations typically reserved for thick-skinned areas and milder preparations used on sensitive regions like the face and skin folds.
These medications should be applied specifically to red, itchy areas during active flare-ups and discontinued once symptoms resolve to prevent unnecessary side effects.
Proper use under medical supervision is crucial to avoid potential complications such as skin thinning, stretch marks, or systemic absorption, particularly with prolonged use of high-potency preparations.
3. Topical Calcineurin Inhibitors (TCIs)
Topical calcineurin inhibitors, including tacrolimus and pimecrolimus, provide effective non-steroidal alternatives for eczema management, particularly in patients who cannot tolerate or have contraindications to corticosteroid use.
These medications are especially effective for maintenance therapy, helping to prevent flare-ups and maintain skin health between acute episodes.
One of the primary advantages of calcineurin inhibitors is their superior side effect profile compared to long-term steroid use, as they do not cause skin thinning or other steroid-related complications.
However, these medications may not provide sufficient anti-inflammatory effect during acute, severe flare-ups and are best suited for mild to moderate symptoms or preventive care.
4. Topical PDE4 Inhibitors
Topical phosphodiesterase-4 (PDE4) inhibitors represent a newer class of non-steroid treatment options, with crisaborole being a prominent example of this therapeutic approach.
These medications offer a valuable treatment option that is suitable for both adults and children as young as 3 months, making them particularly useful for pediatric eczema management where steroid use may be limited.
PDE4 inhibitors work by targeting specific inflammatory pathways involved in eczema, providing effective symptom relief without many of the side effects associated with traditional treatments.
Oral Medications
1. Antihistamines
Oral antihistamines can help relieve the intense itching associated with eczema and may improve sleep quality for patients whose symptoms worsen at night.
These medications work by blocking histamine receptors that contribute to itching and inflammatory responses in the skin.
However, antihistamines are not recommended for long-term use as a primary eczema treatment, as their effectiveness may diminish over time and they do not address the underlying inflammatory process.
2. Antibiotics
Oral antibiotics are specifically prescribed when there is clear evidence of secondary bacterial skin infection complicating eczema, such as increased redness, warmth, pus formation, or systemic signs of infection.
It is essential for patients to complete the full course of antibiotics as prescribed to ensure effectiveness and prevent the development of antibiotic-resistant bacteria, even if symptoms appear to improve before the medication is finished.
3. Oral Steroids
Oral corticosteroids may be prescribed for short-term use during severe eczema flare-ups that do not respond adequately to topical treatments.
These powerful anti-inflammatory medications can provide rapid symptom relief but are not recommended for regular or long-term use due to significant potential side effects including bone thinning, increased infection risk, mood changes, and hormonal disruptions.
4. Immunosuppressants
Systemic immunosuppressant medications are reserved for severe, persistent eczema that has not responded to other treatment approaches.
These medications, such as cyclosporine, require regular monitoring through blood tests and medical examinations due to potential side effects including increased infection risk, kidney problems, and elevated blood pressure.
Despite these concerns, immunosuppressants can be highly effective for patients with debilitating eczema that significantly impacts their quality of life.
Advanced Treatments
1. Phototherapy (UV Light Treatment)
Phototherapy utilizes carefully controlled narrowband UVB light to reduce inflammation and improve eczema symptoms, particularly in patients with extensive disease covering large body areas where topical treatments may be impractical.
This treatment modality requires multiple sessions over several weeks or months and is typically administered in specialized medical facilities under professional supervision.
Patients may experience initial redness and itchiness following phototherapy sessions, similar to mild sunburn, but these effects usually subside as the skin adapts to treatment.
Long-term phototherapy requires careful monitoring for potential skin changes and increased skin cancer risk.
2. Biologics
Biologic medications represent a revolutionary advancement in eczema treatment, with injectable medications like dupilumab specifically designed for severe atopic dermatitis that has not responded to conventional therapies.
These sophisticated medications target specific immune pathways involved in eczema development, providing highly targeted treatment that addresses the underlying disease process.
Biologics generally have minimal side effects compared to traditional immunosuppressants, though they can be costly and may require prior authorization from insurance providers.
Despite the expense, many patients experience dramatic improvement in their symptoms and quality of life with biologic therapy.
3. JAK Inhibitors
Janus kinase (JAK) inhibitors represent a newer class of oral medications for moderate to severe atopic dermatitis, with examples including baricitinib, abrocitinib, and upadacitinib.
These medications work by blocking specific proteins that stimulate immune pathways responsible for eczema inflammation, providing an oral alternative to injectable biologics.
JAK inhibitors offer the convenience of oral administration while providing effective symptom control for many patients with moderate to severe eczema who have not achieved adequate improvement with topical treatments alone.
4. Wet-Wrap Therapy
Wet-wrap therapy involves a specialized technique of applying prescribed medications and moisturizers to affected skin, then wrapping the areas with wet bandages or clothing to enhance medication absorption and provide intensive hydration.
This treatment approach can be particularly effective for severe flare-ups and can often be performed overnight for convenience.
The enhanced medication absorption achieved through wet-wrap therapy can accelerate healing and provide significant symptom relief.
However, this technique should not be used with corticosteroids unless specifically advised by a healthcare provider, as the increased absorption could potentially lead to systemic steroid effects.
Self-Care Strategies for Managing Eczema
Daily Skin Care Routine
1. Bathing Practices
Proper bathing practices are fundamental to eczema management and involve taking short baths or showers lasting no more than 10 minutes using lukewarm water.
- Hot water should be avoided as it strips away the skin’s natural protective oils and can trigger or worsen eczema flare-ups.
- Patients should use gentle cleansers that are specifically formulated to be free from fragrances, dyes, and other potential irritants that can sensitize eczema-prone skin.
- After bathing, skin should be patted dry gently with a soft towel rather than rubbing vigorously, which can cause mechanical irritation and trigger itching or inflammation.
2. Moisturizing
Effective moisturizing requires applying moisturizers liberally at least twice daily, with many dermatologists recommending even more frequent application during flare-ups or in dry climates.
- Patients should choose fragrance-free, hypoallergenic products that have been specifically formulated for sensitive skin conditions.
- The most effective moisturizing occurs immediately after bathing while the skin is still damp, as this timing maximizes moisture retention and enhances the barrier repair properties of the moisturizer.
- Creams or ointments should be chosen over lotions whenever possible, as they provide superior hydration and longer-lasting protection for eczema-prone skin.
3. Trigger Management
Successful eczema management requires patients to identify and systematically avoid their personal triggers through careful observation and, when necessary, formal allergy testing.
- Using protective clothing when handling potential irritants such as cleaning products or gardening materials can prevent direct skin contact that might trigger flare-ups.
- Wearing protective gloves when doing housework helps avoid contact with detergents and other cleaning chemicals that commonly trigger hand eczema.
- Clothing choices should favor soft, breathable cotton fabrics over rough or synthetic materials that can cause mechanical irritation and worsen symptoms.
4. Environmental Controls
Maintaining comfortable room temperature and humidity levels helps prevent the skin dryness that can trigger eczema flare-ups, with ideal indoor humidity levels typically ranging between 30-50%.
- Reducing exposure to dust mites requires frequent cleaning of living spaces, including regular vacuuming, dusting, and washing of bedding in hot water.
- Avoiding carpets, stuffed toys, and other dust collectors in bedrooms and frequently used living areas can significantly reduce allergen exposure.
- Using dust mite-proof covers for mattresses and pillows creates an additional barrier against these common eczema triggers.
5. Stress Management
Psychological stress management plays a crucial role in eczema control, as stress can directly trigger flare-ups through various biological pathways.
- Practicing relaxation techniques such as deep breathing exercises, meditation, or progressive muscle relaxation can help reduce stress-induced eczema symptoms.
- Getting adequate sleep is essential for immune system function and skin healing, while moderate exercise can help manage stress levels and improve overall health.
- However, patients should shower promptly after exercise to remove sweat and prevent irritation.
- Some individuals may benefit from professional counseling if stress significantly affects their eczema management or quality of life.
Special Considerations
For Children with Eczema:
Managing eczema in children requires special attention to age-appropriate skincare practices and safety considerations.
Bubble baths and harsh soaps should be avoided completely, as children’s skin is more sensitive and prone to irritation than adult skin.
Keeping children’s fingernails short and smooth helps minimize damage from scratching, which can lead to secondary infections and scarring.
Cotton clothing and bedding should be used whenever possible to reduce mechanical irritation and improve breathability.
Wet wraps may be considered for severe flares in children, but this should only be done as directed by a healthcare provider who can ensure proper technique and safety.
Parents should work closely with medical professionals to monitor for food allergies, which are more commonly associated with childhood eczema than adult-onset disease.
For Adults with Occupational Exposure:
Adults whose work involves regular exposure to potential irritants require specialized strategies to manage work-related eczema triggers.
Using appropriate protective gear such as gloves, aprons, or protective clothing when working with irritants can prevent direct skin contact that triggers occupational dermatitis.
Hands should be washed with gentle, fragrance-free cleansers rather than harsh industrial soaps, and barrier creams should be applied before exposure to irritants to provide additional protection.
Frequent moisturizing throughout the workday helps maintain skin barrier function and prevent the dryness that can make skin more susceptible to irritants.
In cases where severe occupational dermatitis persists despite protective measures, individuals may need to consider job modifications or workplace accommodations to protect their health and prevent permanent skin damage.
When to Seek Medical Help
While many cases of eczema can be managed with self-care and over-the-counter treatments, you should consult a dermatologist if:
- Your symptoms cause significant discomfort or interfere with daily activities
- Your skin shows signs of infection (redness, warmth, swelling, yellow crust, pus)
- Self-management methods have not improved symptoms after 1-2 weeks
- Your sleep is significantly disrupted by itching
- The affected areas are widespread
- You experience side effects from treatments
- You notice sudden changes in your symptoms
FAQ
What is the difference between eczema and allergies?
Eczema and allergies are two distinct conditions. Allergies typically involve a specific immune reaction to allergens, while eczema is a chronic inflammatory skin condition with various triggers beyond allergens.
However, they often coexist, and many people with eczema also have allergic conditions like asthma or hay fever.
Is eczema contagious?
No, eczema is not contagious. It cannot be spread through any form of contact with an affected person. Eczema develops due to a combination of genetic factors, immune system responses, and environmental triggers.
Can eczema be cured?
There is no definitive cure for eczema. However, with proper management, most cases can be controlled effectively, minimizing flare-ups and improving quality of life.
Many children with eczema see improvement as they grow older, though some may experience recurrence in adulthood.
Does food allergy cause eczema?
Food allergies are linked to eczema in only about 10-15% of cases, primarily in young children.
The most common food sensitivities associated with eczema are milk, wheat, eggs, fish, and nuts.
If you suspect food allergies are triggering eczema, consult a dermatologist for proper testing rather than eliminating foods unnecessarily.
Are topical steroids dangerous for treating eczema?
When used appropriately under medical supervision, topical steroids are safe and effective for treating eczema inflammation.
Risks of side effects like skin thinning are minimal when steroids are used at the correct strength, in appropriate amounts, for limited periods, and on the recommended areas.
Avoiding or delaying steroid treatment when needed can lead to worsening of eczema and potentially require stronger treatments later.
Can I become dependent on topical steroids?
There is no evidence that topical steroids cause dependence or addiction. The need to use steroids repeatedly often results from inadequate treatment of previous flares or underlying persistent inflammation. Following your doctor’s instructions regarding application and duration is important to achieve optimal control.
How does stress affect eczema?
Stress can be a significant trigger for eczema flares. During stressful periods, the body releases chemicals that can increase inflammation and worsen eczema symptoms.
Additionally, stress may lead to scratching behavior that damages the skin barrier. Stress management techniques like meditation, adequate sleep, and regular exercise can help reduce stress-induced flares.
Is it safe to exercise with eczema?
Exercise is generally beneficial for overall health and well-being, but individuals with eczema need to be mindful that sweat can irritate eczema-prone skin and potentially trigger flare-ups.
The salt content and acidic nature of sweat, combined with increased skin temperature during physical activity, can cause stinging, burning, and increased itching in areas affected by eczema.
If you currently have active eczema with red, inflamed, or broken skin, you might want to temporarily reduce exercise intensity or modify your workout routine until symptoms improve and the skin barrier heals.
This doesn’t mean avoiding all physical activity, but rather choosing gentler forms of movement that produce less sweat and heat buildup.
Once your eczema is under control and symptoms have stabilized, swimming in moderation can be an excellent exercise option as the water helps keep your skin cool and may provide soothing relief.
However, swimming requires special precautions to protect eczema-prone skin from potential irritants.
Before swimming, it’s important to apply a barrier cream or petroleum jelly to create a protective layer that shields the skin from chlorine and other pool chemicals that can be highly irritating to sensitive skin.
After any form of exercise, shower promptly to remove sweat, chlorine, and other potential irritants that may have accumulated on the skin during physical activity.
Following the shower, apply moisturizer immediately while the skin is still damp to lock in hydration and restore the skin’s protective barrier.
During exercise, wearing loose, breathable clothing made from soft, natural fabrics helps prevent overheating and allows sweat to evaporate more easily, reducing the time that irritating moisture remains in contact with the skin.
What new treatments are available for severe eczema in Singapore?
Singapore’s healthcare system offers several advanced treatment options specifically designed for severe eczema cases that have not responded adequately to conventional therapies, providing hope for patients who have struggled with persistent symptoms despite standard treatments.
Biologic medications such as dupilumab represent a significant advancement in eczema treatment, as these sophisticated injectable drugs target specific immune pathways involved in the inflammatory process that drives eczema.
Unlike traditional immunosuppressants that broadly suppress the immune system, biologics provide precise targeting of the molecular mechanisms responsible for eczema symptoms.
JAK inhibitors, including baricitinib, abrocitinib, and upadacitinib, offer oral treatment options that block specific proteins responsible for stimulating inflammatory immune pathways.
These medications provide the convenience of oral administration while delivering targeted therapy that can significantly improve symptoms in patients with moderate to severe atopic dermatitis.
Narrowband UVB phototherapy utilizes carefully controlled ultraviolet light exposure to reduce inflammation and improve skin symptoms, particularly beneficial for patients with extensive eczema covering large body areas where topical treatments may be impractical or insufficient.
Topical PDE4 inhibitors like crisaborole provide a newer class of non-steroidal topical treatments that can be used safely in both adults and children, offering an alternative for patients who cannot tolerate or have contraindications to traditional topical corticosteroids.
Modern eczema management in Singapore also emphasizes personalized treatment approaches that combine various therapies tailored to individual patient needs, severity of disease, and response patterns.
These newer treatment options generally offer better efficacy with fewer side effects compared to traditional immunosuppressants, though some treatments, particularly biologics, can be costly and may require insurance pre-authorization or government subsidy programs.
How can I prevent eczema flare-ups?
While you can’t completely prevent eczema if you’re genetically predisposed, you can reduce the frequency and severity of flare-ups by:
Regular moisturizing forms the foundation of eczema prevention and should be performed at least twice daily using fragrance-free, hypoallergenic products that help maintain the skin’s protective barrier function.
This consistent moisturizing routine helps prevent the skin dryness that often triggers eczema symptoms and maintains optimal skin hydration between flare-ups.
Identifying and systematically avoiding known personal triggers is crucial for long-term eczema management, whether these triggers are environmental allergens, specific foods, stress factors, or irritating substances encountered in daily life.
Keeping a detailed symptom diary can help patients and healthcare providers identify patterns and specific triggers that may not be immediately obvious.
Modifying bathing habits by taking quick, lukewarm showers instead of hot baths helps preserve the skin’s natural oils and prevents the excessive drying that can precipitate eczema flare-ups.
Hot water strips away protective lipids from the skin surface, compromising barrier function and increasing susceptibility to irritants and allergens.
Using gentle, fragrance-free cleansers specifically formulated for sensitive skin helps minimize chemical irritation and reduces exposure to potential sensitizing ingredients that can trigger allergic reactions or contact dermatitis in susceptible individuals.
Clothing choices play an important role in prevention, with soft, breathable fabrics like cotton being preferable to synthetic materials or wool that can cause mechanical irritation through friction against sensitive skin.
Loose-fitting garments also help prevent overheating and excessive sweating that can irritate eczema-prone areas.
Effective stress management through relaxation techniques, adequate sleep, regular exercise, and professional counseling when needed helps address the psychological triggers that can significantly impact eczema severity and frequency of flare-ups.
Environmental controls such as keeping living spaces cool and maintaining moderate humidity levels help prevent the excessive dryness or heat that can trigger symptoms, while using air purifiers and dust mite-proof bedding can reduce exposure to common allergens.
Following prescribed treatment plans consistently, even during periods when symptoms are well-controlled, helps maintain remission and prevents minor irritations from developing into full-blown flare-ups.
This includes continuing maintenance moisturizing routines and using prescribed medications as directed by healthcare providers.
Finally, consulting with a dermatologist at the first sign of a flare-up allows for prompt intervention that can prevent symptoms from escalating and becoming more difficult to control, ultimately leading to better long-term outcomes and improved quality of life.
Does eczema affect children and adults differently?
Yes, eczema presents differently depending on age. In babies, it typically affects the face, scalp, and sometimes the body. In older children, it commonly appears in the bends of elbows, behind knees, and on the neck.
Adults may have similar patterns to older children but might also experience more hand, wrist, and facial eczema.
Adults generally have more chronic, persistent disease patterns, while children may experience more fluctuations and potential improvement with age.

